Cervical Spinal Cord Toxoplasmosis in a Patient with AIDS: Case Report and Review of the Literature
Ibrahim Sbeih, Montaser Bilbisi, Rami Darwazeh, Taha Al-gahoom and Hussam Abu-Farsakh
DOI10.21767/2471-9633.10008
1Neurosurgical Department, Ibn Al-Haytham Hospital, Amman, Jordan
2Department of Infectious Diseases, Jordan Hospital, Amman, Jordan
3Pathology Department, First medical Lab, Amman, Jordan
- Corresponding Author:
- Ibrahim Sbeih MBChB, FRCS, FRCS(SN)
Neurosurgical Department
Ibn Al-Haytham Hospital
P.O. Box: 940614, Amman 11194, Jordan
Tel: 600962/795527699
Fax: 0962/6/5516832
E-mail: ibrahimsbeihaz@gmail.com
Received date: February 17, 2016; Accepted date: March 25, 2016; Published date: April 01, 2016
Citation: Sbeih I, Bilbisi M, Darwazeh R, et al. Cervical Spinal Cord Toxoplasmosis in a Patient with AIDS: Case Report and Review of the Literature. Neurosurg. 2016, 1:2. doi:10.21767/2471-9633.10008
Abstract
Background and Importance: Cerebral Toxoplasmosis is a very common cause of focal neurologic disorder in Acquired Immune Deficiency Syndrome (AIDS) patients with cerebral lesions, but it seems to be a rare cause of spinal cord disease. If not treated and detected immediately, Toxoplasmosis may cause considerable mortality and morbidity.
Clinical Presentation: Here we present a case of spinal cord Toxoplasmosis with quadriparesis and acute deterioration that mimicked a neoplasm and resulted in surgical resection.
Conclusion: Detection of enhanced spinal cord lesion in Acquired Immune Deficiency Syndrome(AIDS) patients demonstrate a diagnostic challenge. In these patients, brain imaging, preoperative knowledge of the immune status, serological and cerebrospinal fluid analysis are essential in narrowing the differential diagnosis. All Human Immunodeficiency Virus (HIV) infected patients should be well educated about prophylaxis for Toxoplasmosis infection, and seropositive patients must receive primary or secondary prophylaxis. We carried out a comprehensive review of radiological findings, diagnosis and treatment of this unusual topic.
Keywords
Acquired Immune Deficiency Syndrome (AIDS); Cerebral toxoplasmosis; Human immunodeficiency virus (HIV); Intramedullary spinal cord lesion; Quadriparesis; Spinal cord Toxoplasmosis
Background and Importance
Toxoplasma gondii is an intracellular pathogen that contracts a major proportion of the world population. Also, it is a well-known cause of sickness among persons with Acquired Immune Deficiency Syndrome(AIDS) [1]. Although brain has been the major site for Toxoplasma infection in Acquired Immune Deficiency Syndrome (AIDS) patients, spinal cord involvement by Toxoplasma has been seldom reported. Spinal cord Toxoplasmosis may present as severe outset weakness in both lower limbs correlating with both sensory and bladder dysfunction [2]. On the other hand, progression of cerebral infection may produce seizures, ataxia, confusion, aphasia, hemianopsia, hemiparesis, drowsiness, and cranial nerve palsies [1]. Congenital Toxoplasmosis is an illness caused by intrauterine transmission of the parasite Toxoplasma gondii to the fetus. A pregnant woman may acquire this parasite during gestation. Toxoplasma gondii can be found in up to 50% of the world population [3]. Approximately 10% of patients with Acquired Immune Deficiency Syndrome (AIDS) show some kind of neurological deficit as their primary complaint, and around 80% will have Central Nervous System (CNS) involvement during the course of their illness [1,4,5]. The retina and the lungs are the major sites of extracerebral manifestation of Toxoplasmosis, and such manifestations may happen with/without concomitant Encephalitis [1]. Here we present a case report and review of the literature on Toxoplasmosis in Acquired Immune Deficiency Syndrome (AIDS) patients.
Clinical Presentation
A 40 year old Syrian –married with children- male patient was admitted to our hospital on 26th of November 2005. He gave 18 months history of upper and lower limbs weakness with loss of sensation, urinary retention, chronic constipation and abdominal pain. There was no history of systemic illness, but our patient mentioned having been diagnosed with Herpes Zoster in left arm approximately 4 months prior to admission. The patient was cachectic and his chest examination revealed diffuse harsh breathing sounds and wheezes with crepitation. There were no masses and no organomegaly in his abdomen. Cranial nerves examination revealed left upper motor neuron facial nerve weakness with left eye ptosis. Babiniski sign was positive (up going) on the left side. A Neurological Examination confirmed decreased tone in left upper and lower extremities, reduced power to 3/5 degree in four extremities more on the left side with sensory level at T3. The patient’s hemoglobin level was low (value: 10.8 mg/ dL, normal: 12-16 mg/dL) while platelet levels were high (value: 589*10E9/L, normal: 150-450*10E9/L). Kidney function tests showed an increase in urea, creatinine and potassium levels. ECG revealed normal sinus rhythm within normal limits. Chest x-ray revealed diffuse bilateral infiltration. An abdomen and pelvis ultrasound revealed swelling of the pelvicalyceal system on the right due to distal obstruction. The liver, gall bladder, prostate and left kidney appeared normal. A brain MRI (before and after I.V. injection of Gadolinium) revealed several small rounded lesions scattering in both cerebral hemispheres affecting the right side more than the left (Figure 1).
Figure 1: Preoperative axial brain Magnetic Resonance Imaging
showing multiple enhancing lesions located in the right
internal capsule and Thalamus.
(A) T1 weighted image without contrast showing
isointense lesions. (B) T1 post-contrast image showing
mild enhancement with three small lesions in the right
thalamic area. These lesions appear hyperintense in Flair (C)
and T2 weighted images without significant mass effect (D).
Cervical spine MRI (before and after I.V. injection of Gadolinium) revealed an elongated intra-medullary lesion seen in the cervico-thoracic region starting at the level C1 and ending at the upper level of T4, expanding the spinal cord (Figure 2).
Figure 2: Preoperative sagittal and axial cervical spine
Magnetic Resonance Imaging.
(A) T1 weighted image without contrast showing
isointense lesion. (B) and (D) T1 weighted image
post-contrast showing enhancement in the mid
portion of the lesion extending from C5 till C7-T1
disc space, located left paracentrally in the spinal
cord. (C) and (E) T2 weighted images showing
hyperintense lesion.
The patient denied any history of high risk behavior and there was no history of blood transfusions. He used to have exposure to cats, as home pets.
Surgical exploration was conducted for the aim of lesion resection with the preoperative diagnosis of spinal cord neoplasm. The clinical decision to operate was based on the lesion’s imaging characteristics, including the expansile intramedullary enhancing features and rapid progression of symptoms. He was given 64mg of methylprednisolone 24 and 6 hours preoperatively, and same dose 6 and 48 hours postoperatively. Intraoperatively, patient was put in the semi-sitting position under endotracheal tube and general anesthesia. After routine preparation and toweling, skin incision and laminectomy from C4 till C7 was completed and dural sac was opened. Midline opening of posterior sulcus (Myelotomy) over the whole extent of the lesion was perfomed. We found swollen spinal cord with gliotic and thickened necrotic tissue in the center of the cord. Tough avascular fibrous tissue was found and excised (no plain of cleavage was found and partial excision was achieved). Patient woke up from general anesthesia fully conscious, with Glasgow Coma Scale (GCS) of 15/15.
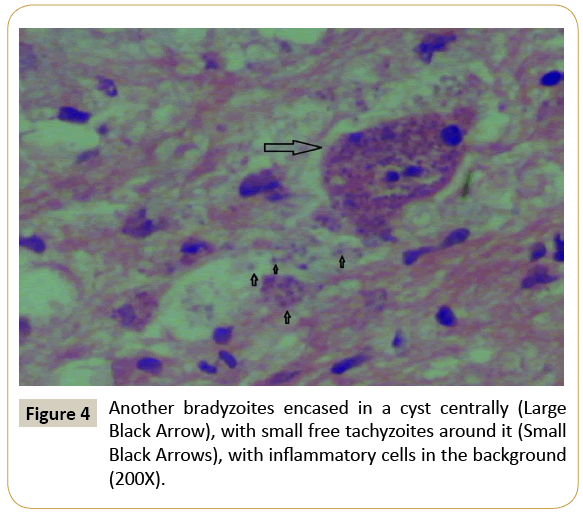
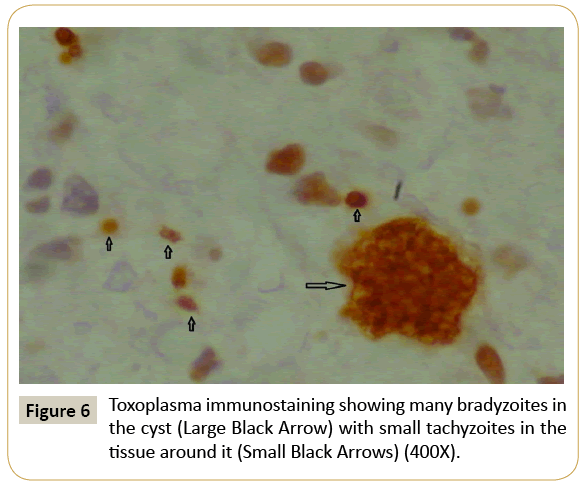
Histopathological sections show glial tissue with inflammatory cells in the background and few encased cysts. These cysts represent the latent form of Toxoplasma by slow-growing protozoa forms called bradyzoites encased in cysts with a cyst wall. Multiple basophilic dot-like parasites could be seen in cysts. The Toxoplasma cysts show true cystic wall, but may be incorrect for necrotic cell debris, (Figure 3). In active disease, inflammatory cells may border the cyst. Active parenchyma glial tissue disease is recognized by the appearance of tachyzoites, which are free parasites in the tissue and which induce an inflammatory response (Figures 4 and 5). Transformation of bradyzoites to tachyzoites takes place during immunosuppression. Tachyzoites described as crescent-shaped 4-8 microns large organisms with a nucleus that clearly invade into the neuropil. As a result, the patient symptoms may be caused by a mixed inflammatory reaction. Immunohistochemistry stains were performed to confirm the Toxoplasma organisms and it was positive in both forms (bradyzoites and tachyzoites) (Figure 6).
On 4th postoperative day, his Anti-Toxoplasma Immunoglobulin (IgG) titer was positive at 3.44 IU/mL (Positive >1.01 IU/mL). Human Immunodeficiency Virus (HIV) Antibodies by ELISA were positive with positive western blotting results, confirmed a diagnosis of Human Immunodeficiency Virus (HIV). Human Immunodeficiency Virus (HIV) RNA by Polymerase Chain Reaction (PCR) was 2.19*107 virus /mL (Negative viral load, range: <400). The patient was started on Antitoxoplasma therapy in the form of: Bactrim (sulfamethoxazole 800 mg + trimethoprim 160 mg, AR Scientific, Inc., forte, two tablets by mouth twice daily) for 8 weeks and Daraprim (Pyrimethamine, Amedra Pharmaceuticals LLC ,200 mg tablet by mouth loading dose followed by 75 mg by mouth once daily) for 8 weeks along with (HAART) therapy; Regimen used was Combivir (Zidovudine 300 mg + Lamivudine 150mg, GlaxoSmithKline, one tablet by mouth twice daily) for 8 weeks, Kaletra (Lopinavir , AbbVie, Inc. ,200 mg tablet, three tablets by mouth twice daily) for 8 weeks, Norvir (Ritonavir, AbbVie, Inc., 600 mg, one tablet by mouth twice daily ) for 8 weeks, Dalacin (Clindamycin, Pfizer Ltd., 600 mg Vial, Intravenous (IV) Q6hrs) for 8 weeks and Becozym forte (Vitamin B complex, Piramal Healthcare, three tablets by mouth daily) for 8 weeks. He was maintained on Bactrim (sulfamethoxazole 800 mg+trimethoprim 160 mg, AR Scientific, Inc., forte, two tablets by mouth twice daily) for secondary prophylaxis for another 4 weeks.
Post-operative MRI one week after surgery revealed subtotal resection of the lesion (Figure 7). The patient’s stay in the ward was uneventful and he made a smooth recovery. He was discharged on the 9th post-operative day. Clinical recovery was noticed with partial recovery of his neurological functions.
Follow-up consisted of a spinal cord and brain MRI (with and without Gadolinium) on December 2005 (1 month postoperatively), February 2006 (3 months postoperatively), July 2006 (8 months postoperatively) and July 2010 (56 months postoperatively) respectively (Figure 8). Brain lesions improved and disappeared and spinal cord swelling resolved (Figure 9). Human Immunodeficiency Virus (HIV) RNA by Polymerase Chain Reaction (PCR) was undetectable. After June 2013 it was difficult to follow up the patient because of War in his home country, Syria. Last phone contact with him was in June 2014 (103 months postoperatively) when he reported being well, leading a normal life.
Figure 8: A follow up Magnetic Resonance Imaging of cervical spine showing disappearance of spinal intramedullary lesion. Cervical cord looks thin and angulated. (A) 3 months postoperative Magnetic Resonance Imaging (B) 8 months postoperative Magnetic Resonance Imaging (C) 56 months postoperative Magnetic Resonance Imaging (D) 91 months postoperative Magnetic Resonance Imaging.
Discussion
Toxoplasma gondii is an intracellular protozoan that generally presents in patients with Acquired Immune Deficiency Syndrome (AIDS) as reactivation of latent infection [6]. It is typically latent and remains asymptomatic in both Human Immunodeficiency Virus-infected patients and immunocompetent individuals [1]. It is considered as a very common cause of intracranial abscesses in HIV/AIDS patients but appears to be an infrequent cause of spinal cord disease [4]. The incidence of Toxoplasmosis in adult in USA range from 20%-70%, the two major routes of transmission of Toxoplasmosis to humans are oral and congenital [5]. A literature review mentions that although Toxoplasmosis is infrequent, it have to be suspected in immunocompromised patients who present with symptoms of acute or sub-acute myelopathy [4].
Patients with cerebral Toxoplasmosis may present with altered mental status (62%), fever (41%), or headaches (59%) associated with focal neurologic deficits [1]. Although spinal cord Toxoplasmosis is infrequent, it has been mentioned that most patients with Acquired Immune Deficiency Syndrome (AIDS) that present with progressive myelopathy, characterized by spinal cord swelling, sensory involvement, extremity weakness, enhancing lesions in spinal cord or brain on CT or MRI, have Toxoplasmic Myelitis [4]. This may or may not be associated with brain involvement [6].
In approaching a single intramedullary spinal lesion, a set of laboratory tests and imaging may help narrow the differential diagnosis and in some cases, help establish the diagnosis.
Toxoplasma gondii infection is generally detected by performing serologic studies for antitoxoplasma antibodies. The serum IgG Antitoxoplasma titer peaks between 1 and 2 months after primary infection and often remains detectable for the rest of the patient’s life. Generally, serum assays should not be used as the single diagnostic study for active Toxoplasmosis, these studies alone cannot differentiate latent from active infection. Nevertheless, in patients with known baseline Antitoxoplasma IgG levels, an elevation in the IgG level during the presence of symptoms may point out reactivation of Toxoplasmosis. A negative serologic test for IgG makes the diagnosis of reactivated Toxoplasmosis less likely, and other causes of focal neurologic deficits should be included in the differential diagnosis [1]. However, negative IgG serology should not exclude Toxoplasma infection, as patients with Advanced Human Immunodeficiency Virus (HIV) infection may turn seronegative. IgM Antitoxoplasma antibodies usually disappear within weeks to months after the primary infection but may remain elevated for more than 1 year. Because antitoxoplasma IgM antibodies typically are absent in patients with reactivated disease and Toxoplasmic Encephalitis in Human Immunodeficiency Virus-infected patients is most often due to reactivated disease, the IgM antibody test is usually not useful in the workup for cerebral Toxoplasmosis.1 In patients with Acquired Immune Deficiency Syndrome (AIDS), Toxoplasmosis generally reactivates when the CD4+ cell count drops below 100/ μL [6]. Analysis of Cerebrospinal fluid (CSF) is scarcely useful in the diagnosis of Toxoplasmosis [1,2,6]. It may be used for the confirmation of diagnosis but should not be used for exclusion of diagnosis [1,2].
The clinical presentation of neoplastic and non-neoplastic spinal cord lesions may be similar, and MRI is useful for making an accurate diagnosis. Typical MRI finding in Toxoplasmic Myelitis consists of intramedullary ring enhancing lesion in the affected area. Other disorders which can present with similar findings include Primary Central Nervous System Lymphoma (PCNL), Tuberculoma, Neurocysticercosis or rarely abscess due to Streptococcus, Staphylococcus, Aspergillus, Salmonella, Rhodococcus, or Nocardia [2]. Other causes of myelopathy in Human Immunodeficiency Virus (HIV) patients include bony lesions, epidural abscess, Cytomegalovirus Polyradiculitis, Herpes Myelitis, Lymphoma, Tuberculoma or Human Immunodeficiency Virus (HIV) vacuolated myelopathy [2]. In Cerebral Toxoplasmosis one might see the asymmetric target sign, which represents a ring-enhancing abscess seen in both Computed Tomography and Magnetic Resonance Imaging. A noncontrast Computed Tomography scan may detect a hypodense lesion in the brain that can be mistaken for other types of focal brain lesions; however, a repeat Computed Tomography scan with contrast will demonstrate the typical ring-enhancing sign [1]. On T1-weighted MRI, toxoplasmic lesions are typically isointense in relation to the rest of the brain tissue [7]. On T2-weighted MRI, the lesions are generally hyperintense. Diffusion Weighted Imaging (DWI) may be helpful in excluding of Lymphoma which shows no restriction in water diffusion [4].
Other potentially useful imaging modalities include Positron Emission Tomography (PET); we found 1 case report in the literature with Positron Emission Tomography (PET) presentation seen in the form of transverse myelitis. Another case report showed an enhancing intramedullary lesion on MR imaging and concomitant increased metabolic activity on the Positron Emission Tomography (PET) scan, simulating a tumor [8]. Single Photon Emission Computed Tomography (SPECT) may be helpful for differentiating Toxoplasmic Encephalitis from Central Nervous System (CNS) lymphoma [1].
Non-infectious differential diagnosis in Human Immunodeficiency Virus patients with multiple ring-enhancing lesions on Computed Tomography or Magnetic Resonance Imaging include primary central nervous system lymphoma, primary brain tumors (rarely Glioblastoma), brain metastasis, demyelinating diseases (e.g.: Multiple Sclerosis). Lymphoma is considered as a primary intramedullary spinal cord lesion [8]. Neuroimaging findings, along with other clues, help to narrow the differential diagnosis. Concerning inflammatory lesions such as neurosarcoidosis, the lack of brain and spinal leptomeningeal enhancement and multifocal patchy cord enhancement decreases the diagnostic possibility of neurosarcoidosis [8]. Other intamedullary lesion that may mimick a neoplasm is localized Multiple Sclerosis (MS). Multiple Sclerosis (MS) is characterized by various areas of demyelination and sclerosis in Central Nervous System (CNS). The histological specific aspects of Multiple Sclerosis (MS) are demyelinating lesions with total of foamy histiocytes. In our case the probability of Multiple Sclerosis (MS) lesion was excluded because the lesion did not have these histological aspects and there was no evidence of demyelinating lesions in other areas. Other lesion which may mimick an intramedullary neoplasm is radiation melyopathy. Chronic Progressive Radiation Myelopathy (CPRM) is the most common presentation of this disease, that usually appears 15-20 months after radiation therapy [9]. As for Vasculitides, such as lupus myelitis, a negative serology, absence of white matter lesions in the brain, and multiple spinal cord lesions with patchy enhancement would have helped to mitigate this diagnosis [8]. Moreover degenerative diseases may mimick intramedullary neoplasms caused by contrast uptake of the myelopathy [9]. These lesions may cause considerable difficulties in the differential diagnosis.
Brain biopsy is highly sensitive for diagnosing cerebral lesions, however it carries a considerable risk of hemorrhage and an increased mortality (2%) and morbidity rate (12%) in patients with HIV/AIDS [4]. Also, availability of noninvasive methods such as imaging techniques and serology has led to recommendation of biopsy only when the diagnosis is unclear or if the patient either does not respond to or worsens with tentative treatment [1,6,10].
Histologically, Toxoplasmosis presents either as an acute necrotizing lesion with abundant free organisms (tachyzoites) in addition to parasitic cysts (also known as pseudocysts, corresponding to a macrophages laden with Toxoplasma gondii), as a latent infection (cysts/ bradyzoites in intact tissue), or as a combination of both. Edema and inflammatory infiltrates by lymphocytes with perivascular cuffing will be seen surrounding spinal cord or brain tissue. Macroscopically spinal Toxoplasmosis lesions appear as relatively well-demarcated zones of necrosis with or without hemorrhage [8]. Special tests for infective pathologies are helpful for diagnosis, but histological examination is fundamental for establishing a clear diagnosis [9]. In fact, in the setting of hematological malignancy patients receiving high dose chemotherapy, cerebral Toxoplasmosis is one of the neurologic complication and is related to a high mortality rate [11].
As for treatment, the first line for Toxoplasmic Encephalitis in Acquired Immune Deficiency Syndrome (AIDS) patients consist of combination of Pyrimethamine (200 mg of loading dose, 50 mg/day) and sulfadiazine (4-6 g/day) in addition to folinic acid (10-25 mg/day) [2]. The combination of pyrimethamine and clindamycin may be used as alternative to pyrimethamine and sulfadiazine in patients who experience side-effects or who are allergic to sulfa drugs: but it has been connected to increase relapse rate during the maintenance phase of treatment [12]. In our case, Sulfadiazine was not available and Sulfamethiazole was used instead.
In patients whose clinical condition deteriorates during the first 48 hours of treatment or there is a radiologic evidence of midline shift or signs of increased intracranial pressure, corticosteroid therapy should be considered. Dexamethasone (4 mg every 6 hr) is the most commonly administered agent, and it is tapered over the next few days [7]. Radiological improvement is seen in about 80% of patients, and clinical improvement noticed in about 1 week, supporting the diagnosis [4]. Steroids must be used cautiously in patients with Human Immunodeficiency Virus infection, as these drugs may mask different opportunistic infections.
Screening for Antitoxoplasma IgG antibodies should be completed the moment a patient is diagnosed with Human Immunodeficiency Virus (HIV) in order to estimate the risk for developing acute Toxoplasmosis. All Human Immunodeficiency Virus (HIV) infected patients should be educated about appropriate food handling and willingness to avoid infection with Toxoplasma gondii regardless of serostatus. Patients should be told to wash hands before and after touching uncooked or undercooked meat as well to wash fruits and vegetables well before consumption and to eat only well cooked meat. Eventually, all Human Immunodeficiency Virus (HIV) diagnosed patients should be educated about primary and secondary medical prophylaxis for Toxoplasma gondii infection.
Conclusion
The differential diagnosis of intramedullay spinal cord lesions is wide and may be difficult to assess. We present an undiagnosed patient with Acquired Immune Deficiency Syndrome (AIDS) that presented with Toxoplasmosis and Intramedullary spinal cord lesion, successfully treated with partial resection, Anti Toxoplasma and Antiretroviral medical therapy.
Most patients with Acquired Immune Deficiency Syndrome (AIDS) that present with progressive myelopathy, characterized by spinal cord enlargement, sensory involvement, extremity weakness, and enhancing lesions in spinal cord or brain MRI, have Toxoplasmic Myelitis. The likelihood of this diagnosis is even greater if there are positive serology for Toxoplasmosis or the initiation of early treatment with empiric anti-toxoplasmosis therapy and steroids improves both the patient’s radiographic and clinical manifestations.
Testing for HIV-Antibodies by ELISA must be routinely done preoperatively.
Preoperative MRI may not give a certain diagnosis because of different lesions which have an identical signal intensity pattern. Histological examination is predominantly fundamental for establishing the diagnosis. In this case the worsening of symptoms necessitated an early decompressive surgical strategy in order to achieve a quick improvement and avoid catastrophic permanent sequelae.
Altogether, this case highlights that knowing patient’s immune status is critical. Toxoplasmosis must be kept in mind for differential diagnosis in HIV/AIDS patients. Physician should keep in mind this unusual entity while treating Human Immunodeficiency Virus (HIV) patients presenting as myelopathy.
Conflict of interest
None.
Acknowledgment
The authors gratefully acknowledge Neurosurgery department in Ibn Al-haytham hospital, Infectious disease department at Jordan hospital, and Pathology department, First medical lab - Amman - Jordan.
References
- Jayawardena S, Singh S, Rumyantseva O, Clark H (2008) Cerebral Toxoplasmosis in Adult Patients with HIV Infection 17-24.
- Agrawal SR, Singh V, Ingale S, Jain AP (2014) Toxoplasmosis of spinal cord in acquired immunodeficiency syndrome patient presenting as paraparesis: A rare Entity. J Glob Infect Dis 6:178-181.
- Burrowes D, Boyer K, Swisher CN,Noble AG, Sautter M, et al. (2012) Spinal Cord Lesions in Congenital Toxoplasmosis Demonstrated with Neuroimaging, Including Their Successful Treatment in an Adult. J Neuroparasitology3.
- Levy RM, Bredesen DE, Rosenblum ML (1985) Neurological manifestations of the acquired immunodeficiency syndrome (AIDS): experience at UCSF and review of the literature. J Neurosurg 62: 475-495.
- Garcia-Gubern C, Fuentes CR, Colon-Rolon L, Masvidal D (2010) Spinal cord toxoplasmosis as an unusual presentation of AIDS: case report and review of the literature. Int J Emerg Med. 3: 439-442.
- Arshad S, Skiest D, Granowitz EV (2009)Subacute Onset of Paralysis in a Person with AIDS. AIDS Read.19:32-35.
- Thurnher MM, Post MJ, Jinkins JR (2000) MRI of infections and neoplasms of the spine and spinal cord in 55 patients with AIDS. Neuroradiology 42: 551-563.
- Sidani C, Bhatia R, MJD Post (2013) Underdiagnosed and rare toxoplasma gondii spinal cord lesion simulation cord neoplasm. Neurographics3: 203-207.
- Landi A, Di Norcia V, Dugoni DE, Tarantino R, Cappelletti M, et al. (2010) Intramedullary non-specific inflammatory lesion of the thoracic spine: A case report. World J SurgOncol 8: 3.
- Rodríguez C, Martínez E, Bolívar G, Sánchez S, Carrascal E (2013) Toxoplasmosis of the spinal cord in an immunocompromised patient case report and review of the literature. Colomb Med (Cali) 44: 232–235.
- De Bonis P, Cingolani A, Pompucci A, Tartaglione T, Larocca LM, et al. (2011) CaudaEquina Enhancing Lesion in an HIV-Infected Patient. Case Report and Literature Review. Mediterr J Hematol Infect Dis 3: e2011042.
- Katlama C, De Wit S, O’Doherty E, Van Glabeke M, ClumeckN (1996) Pyrimethamine-clindamycin vs. pyrimethamine-sulfadiazine as acute and long-term therapy for Toxoplasmic Encephalitis in patients with AIDS. Clin Infect Dis 22: 268-275.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences