The Effect of Preoperative Anxiety and Depression on the Clinical Consequences of Discectomy in Rahnemoun Hospital, Yazd, 2020-2022
1Department of Neurosurgery, Yazd University of Medical Sciences, Iran
2Department of Anesthesiology, Yazd University of Medical Sciences, Iran
3Department of General practitioner, Tehran University of Medical Sciences, Iran
- *Corresponding Author:
- Amin Jesmani, Department of Neurosurgery, Yazd University of Medical Sciences, Iran, Tel: 09118997053; E-mail: aminjesmani999@gmail.com
Received date: January 03, 2022, Manuscript No. IPJNCS-22-12578; Editor assigned date: January 05, 2022, PreQC No. IPJNCS-22-12578 (PQ); Reviewed date: January 19, 2022, QC No. IPJNCS-22-12578; Revised date: March 07, 2022, Manuscript No. IPJNCS-22-12578 (R); Published date: March 15, 2022, DOI: 10.36648/2471-9633/22.06.001
Citation: Jesmani A, Ziaee E, Abdollahi MH, Gholizadeh M (2022) The Effect of Preoperative Anxiety and Depression on the Clinical Consequences of Discectomy in Rahnemoun Hospital, Yazd, 2020-2022. Neurosurg Vol:6 No:3
Abstract
Introduction: The consideration of psychological characteristics and their impact on an operation's clinical results can reduce pain for patients, improve the quality of the operation, and increase satisfaction for service recipients. This study examines the relationship between preoperative anxiety and depression for a discectomy and clinical outcomes.
Methodology: As a prospective study, this study was performed among patients referred to the Rahnemoun Hospital of Yazd University of Medical Sciences in 2020 and 2022. Two neurosurgeons at the center diagnosed them with lumbar disc herniation and admitted them to the neurosurgery ward for discectomy. Each patient completed the Orebro Musculoskeletal Pain Questionnaire (OMPQ), Visual Analog Scale (VAS), Oswestry Disability Index (ODI), Hospital Anxiety and Depression Scale (HADS), and the SF-36 Quality of Life Questionnaire the day before discectomy. The above questionnaires were filled out at intervals of two weeks, two months, and six months following discectomy. Data were analyzed using SPSS.
Results: An analysis of the Hospital Anxiety and Depression Scale (HDAS) results in the study patients, based on the ODI questionnaire before surgery, two weeks, two months, and six months after surgery, reveals a significant difference (p 0.05). Further, the results of the Orebro Musculoskeletal Pain Questionnaire (OMPQ) in the studied patients, based on the ODI questionnaire, before surgery, two weeks, two months, and six months after surgery, did not show any significant differences (p>0.05).
Conclusion: According to the results of this study, it can be concluded that the rate of depression and anxiety, physical function, and other patients' psychological variables can be improved after surgery.
Keywords
Anxiety; Depression; Surgery; Discectomy; Clinical outcomes
Introduction
Back pain is one of the most common health problems that people experience throughout their lives, and it has a variety of social and economic effects [1,2]. Following cardiopulmonary disease, low back pain is the second most common reason to visit a doctor, the fifth most common reason for hospitalization, and the third most common reason for surgery. An annual incidence of 5% is estimated, and its prevalence ranges from 0.8% to 82.5% (with a mean of 38.1% and a median of 37.4%). In the United States, 80% of people experience low back pain during their lifetime [3-5], and 3% of them need surgery [6,7]. 51% of people in Iran suffer from low back pain [8].
The most significant clinical manifestation of low back pain is radicular pain in the lower extremities. Typically, the pressure on the nerve root is caused by a herniated lumbar disc [9]. The annual incidence of lumbar disc herniation has been reported to increase by 3.7% for women and 5% for men over 30 years of age, approximately 90 to 97% of all disc herniations occur at the L5-L4 and L5-S1 [10,11]. These patients' symptoms include low back pain, radicular pain in the lower extremities, weakness of the limbs, and sensory-motor disorders [10]. Lumbar disc herniation can be treated with supportive care or by symptomatic treatment, and when necessary, with surgery [12]. 70% of patients with lumbar disc herniation recover within four weeks with supportive care. Nevertheless, surgery will be required if the pain from a herniated lumbar disc is severe and intolerable or if a nerve defect is present [13,14]. A discectomy is widely recognized as a standard surgical procedure for treating lumbar disc herniation [15]. Discectomy is the surgical removal of a part of an intervertebral disc to remove the herniation and reduce the nerve roots or spinal cord [16,17].
Study participants who underwent discectomy five years after surgery had a higher quality of life than those with lumbar disc herniation who used non-surgical procedures [18,19]. Although there are no accurate numbers on the proportion of patients who undergo discectomy, evidence shows that only 70% of them are able to return to work within 12 months. The average success rate of discectomy is 67%, and the average reoperation rate is 10% [20]. An additional study found a success rate of 65%-75% and a reoperation rate of 23%, respectively [21].
Growing evidence indicates that psychological factors may play a role in spinal surgery outcomes [22]. Anxiety and depression are ranked among the most important psychological factors are related to these outcomes [23]. The most common emotion that people experience is anxiety, an unpleasant mental state or situation that is only subjectively threatening or anticipates an unknown threat for one or others [24]. The individual feels uneasy, unbalanced, and under pressure in this state [25]. Anxiety, in and of itself, delays recovery [26]. The condition of depression is characterized by heartburn, despair, and fatigue and is often accompanied by more or less severe anxiety [27]. In addition, it is a long-lasting disorder with specific symptoms that negatively affect performance and anxiety [28]. Surgical procedures increase anxiety and depression in patients and affect their needs and compatibility. Anxiety leads to physiological and psychological changes, changes in thinking, feelings, behaviors, and delays in postoperative recovery, and disturbs the physical, mental, and social human balance [29]. Twenty-three million people undergo surgery each year; most experience preoperative anxiety [30].
In hospitalized patients, anxiety and depression are present between 20 and 60% of the time [31-33] and are not detectable in two-thirds of the patients [34]. Anxiety and depression occur in 11 to 80% of adults during illness and before surgery but do not manifest themselves [35]. Preoperative anxiety and depression are diagnosed by patient assessment, and their severity varies. The effects of preoperative anxiety and depression on patient function are physiologically and psychologically significant [31]. Anxiety and depression before surgery can have adverse psychological and physiological effects [32].
Evaluating anxiety and depression before spinal surgery is critical because it impacts surgical outcomes. Many studies have documented the importance of preoperative anxiety and depression in patients undergoing spinal surgery [36,37]. Junge et al. found that preoperative psychological conditions may help predict poor postoperative clinical outcomes [38,39]. Other studies support these findings.
Examining psychological characteristics and their impact on clinical outcomes
Consequences can reduce patient pain, improve the quality of services, and increase patient satisfaction. Knowing more about this can be helpful for service providers and policymakers in clinical management, on the one hand, and patients and recipients of services, on the other. Therefore, the purpose of the study is to examine the effect of preoperative anxiety and depression on the clinical outcomes of discectomy in Rahnemoun Hospital.
Materials and Methods
Study population
This study was performed as a prospective study among patients referred to the Rahnemoun Hospital of Yazd University of Medical Sciences in 2020 and 2022. Neurosurgeons at the center diagnosed them with lumbar disc herniation and recommended discectomy. A random sample of 81 people was chosen for this study. Among the inclusion criteria for this study are the ages of 18-60 years, confirmation of lumbar disc herniation by MRI, failure of conservative-drug treatment (analgesics and NSAIDs) for at least six weeks, intractable pain or neurological deficit, determining the indication for surgery by two neurosurgeons, discectomy and nerve decompression surgery, and informed consent. Exclusion criteria include the history of psychiatric illness, history of musculoskeletal diseases (fibromyalgia, osteoarthritis, osteoporosis), history of chronic comorbidities such as diabetes, rheumatoid arthritis, instability in the vertebrae in need of fixation, disc herniation, recurrent disc surgery, nerve root resection during surgery, lower extremity paralysis, congenital disease, history of corticosteroid use in 1 month before surgery, and 6-month follow-up period, emergency surgery, history of spinal surgery, postoperative infection, each incident resulted in patient's physical and mental a change after surgery, and neck or thoracic pain during the study period, BMI> 30 or BMI <18, and pregnancy.
Data collection method
After identifying and selecting eligible patients to enter the study and signing the consent one day prior to discectomy, the Örebro Musculoskeletal Pain Questionnaire (ÖMPQ), Visual Analog Scale (VAS), Oswestry Disability Index (ODI), Hospital Anxiety and Depression Scale (HADS), and the SF-36 Quality of Life Questionnaire were completed by each patient. After discectomy, patients were followed for six months, and within two weeks, two months, and six months after discectomy, the VAS and ODI pain questionnaires and the SF-36 quality of life questionnaire were completed again. After completing the questionnaires, data were analyzed by SPSS.
Hospital Anxiety and Depression Scale (HADS)
The questionnaire is widely used to assess patients' anxiety and depression on medical wards and differentiate between patients' psychological and physical aspects. It is designed to assess mood changes, such as anxiety and depression. There are seven questions on anxiety symptoms (questions 1, 4, 5, 8, 9, 12, and 13) and seven questions on depressive symptoms (questions 2, 3, 6, 7, 10, 11, and 14). Scores of 11 or higher are considered clinically significant by the authors. The high scores on the depression scale suggest that other treatments should be considered in addition to anxiety treatment. There are two high-risk groups for this study, defined as people with scores equal to or greater than 11 and two low-risk groups, defined as people with scores below 11. Validity (face, content, simultaneously based on external criteria, convergence, and differentiation) was evaluated.
Örebro Musculoskeletal Pain Questionnaire (ÖMPQ)
The OMPQ questionnaire is used to assess and predict long-term disabilities and failure to return to work due to personal or work-related factors. These factors can be changed or managed through interventions and health care and modify the scores of this questionnaire; therefore, clinicians use it to measure the intervention accuracy. The score ≤ 105 indicates low risk, 105-130 indicates moderate risk, and the score ≥ 130 indicates high risk.
Visual Analog Scale (VAS)
The visual analog scale of pain intensity is a 10 cm ruler, with the word painless written on the left end and the word most severe pain on the right end. The person marks the continuum according to his/her pain in the last 48 hours.
Oswestry Disability Index (ODI)
Researchers and disability assessors use the Oswestry Disability Index (ODI) to measure a person's level of disability. The questionnaire includes ten topics: pain intensity, lifting, self-care ability, walking ability, sitting ability, sexual function, standing ability, social life, sleep quality, and travel ability. Each topic contains six sentences, which describe a potentially different scenario in the patient's life. The patient then chooses the sentence that best describes his or her status. Each question has a scale of 0-5, so that the first sentence or scenario has a score of 0 and indicates the lowest degree of disability, and the score of the last sentence is 5, which indicates the most severe disability. After the scores of all the answered questions are summed, the index (0-100) is doubled. The scores are as follows: 0-20: minimal disability, 21-40: moderate disability, 41-60: severe disability, 61-80: unpleasant pain, and 81-100: patient in bed with severe symptoms.
SF-36 quality of life questionnaire
This questionnaire, which contains 36 questions, examines the health status of individuals and its questions measure eight primary constructs related to personal health, which include four constructs of physical health and four mental health’s constructs. Each subscale consists of two to ten items. Physical Function (PF), Role-Physical (RP) disorder, Role Emotional (RE) disorder, Energy/Fatigue (EF), Emotional Well-Being (EW), Social Function (SF), Pain (P), and General Health (GH) are the eight subscales of this questionnaire. In addition, two general subscales, namely physical health and mental health, are derived from the integration of subscales. Each question has a score between 0 (lowest score) and 100 (highest score), which is assigned to an individual based on the answers to the question options, and the score obtained from the sum of the individual scores to the questions in each structure. A lower score indicates a lower quality of life in this questionnaire and vice versa.
As the data analysis method in this study, linear regression was used to investigate the effects of preoperative anxiety and depression on postoperative outcomes. This study and the regression test had significant levels of 0.05 and 0.01, respectively. Data were analyzed using SPSS 21.
Results
This study was performed on 80 patients who were candidates for discectomy, among which 52 (65%) were male, and 28 (35%) were female. The age means, and standard deviation was
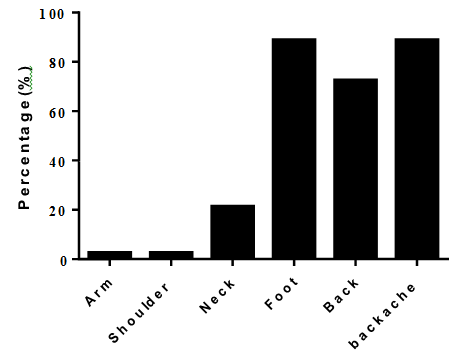
51.96 ± 11.14 years. In this study, the frequency of studied patients was examined in terms of pain location, and the results are reported in Figure 1.
In this study, the mean and standard deviation of HADS for anxiety and depression was 10.57 ± 1.94 and 10.65 ± 2.01, respectively. The mean and standard deviation of the OMPQ in patients was 106.37 ± 8.42. In this study, ODI and SF-36 quality of life subscales were examined at four intervals (before, two weeks, two months, and six months after surgery), the results of which are reported in Table 1.
Table 1: Mean and standard deviation of ODI and SF-36 quality of life subscales.
| Variables | Before | After 2 weeks | After 2 months | After 6 months |
|---|---|---|---|---|
| ODI | 76.72 ± 13.01 | 40.22 ± 14.73 | 26.90 ± 18.37 | 15.00 ± 19.35 |
| Sub-scale of SF-36 | ||||
| Physical function | 13.43 ± 16.12 | 56.93 ± 23.74 | 71.81 ± 25.76 | 79.53 ± 26.60 |
| Limitations due to physical health | 82.50 ± 24.96 | 39.68 ± 29.68 | 24.37 ± 30.02 | 18.12 ± 26.97 |
| Limitations due to emotional health problems | 50.00 ± 40.73 | 31.66 ± 37.83 | 24.16 ± 33.11 | 23.79 ± 32.31 |
| Energy and vitality | 48.62 ± 11.44 | 55.32 ± 12.12 | 60.87 ± 14.00 | 63.62 ± 15.13 |
| Emotional health | 50.40 ± 10.84 | 57.55 ± 11.10 | 61.90 ± 13.07 | 65.75 ± 14.96 |
| Social functions | 31.71 ± 13.18 | 46.25 ± 13.40 | 53.28 ± 17.87 | 63.90 ± 19.48 |
| Pain | 24.90 ± 9.04 | 44.78 ± 15.25 | 55.78 ± 20.98 | 63.56 ± 23.18 |
| General health | 43.56 ± 16.89 | 54.81 ± 16.97 | 60.62 ± 21.03 | 64.50 ± 25.11 |
In this study, the frequency of patients was evaluated considering HDAS. According to the results, 41 patients (51.2%) were low risk (score <11), and 39 patients (48.8%) were high risks (score ≥ 11).
This study examines patients' physical health relationships at different intervals in terms of OMPQ. According to the results, there is no significant relationship between physical healths.
In patients based on OMPQ (P=0.166). Moreover, patients' mental health relationships have been examined at different time intervals according to the Hospital Anxiety Scale (HDAS) questionnaire, which the results show there was no significant relationship between mental health in terms of HDAS (P=0.625).
This study examined the relationship between HDAS questionnaire in the studied patients, in terms of physical health (Table 2), and the relationship between the OMPQ in the studied patients in terms of physical health (Table 3), and the relationship between the OMPQ questionnaire in the studied patients in terms of mental health (Table 4), at different time intervals, and their results are reported in detail in Tables.
Table 2: Relationship between Hospital Anxiety Scale (HDAS) questionnaire in patients in terms of physical health at different time intervals.
| Hospital Anxiety Scale (HDAS) questionnaire | Mean ± Stdv | P value | |
|---|---|---|---|
| People at low risk (with a score below 11) | physical health-before | 42.53 ± 8.58 | <0.001 |
| physical health-after 2 weeks | 53.15 ± 8.46 | ||
| physical health-after 2 weeks | 53.15 ± 8.46 | <0.001 | |
| physical health-after 2 months | 58.32 ± 6.89 | ||
| physical health-after 2 months | 58.32 ± 6.89 | <0.001 | |
| physical health-after 6 months | 62.65 ± 9.05 | ||
| physical health-before | 42.53 ± 8.58 | <0.001 | |
| physical health-after 6 months | 62.65 ± 9.05 | ||
| People at high risk (with a score below 11) | physical health-before | 39.59 ± 6.81 | <0.001 |
| physical health-after 2 weeks | 44.74 ± 10.32 | ||
| physical health-after 2 weeks | 44.74 ± 10.32 | 0.02 | |
| physical health-after 2 months | 47.70 ± 12.03 | ||
| physical health-after 2 months | 47.70 ± 12.03 | 0.154 | |
| physical health-after 6 months | 49.88 ± 13.06 | ||
| physical health-before | 39.59 ± 6.81 | <0.001 | |
| physical health-after 6 months | 49.88 ± 13.06 | ||
Table 3: Relationship between Orebro Musculoskeletal Pain Questionnaire (OMPQ) in patients in terms of physical health.
| Orebro Musculoskeletal Pain Questionnaire (OMPQ) | No. | Mean | Standard deviation |
P value. | |
|---|---|---|---|---|---|
| Lowrisk | physical health-before | 36 | 39.2 | 6.67 | |
| physical health-after 2 weeks | 36 | 48.36 | 7.8 | <0.001 | |
| physical health-after 2 weeks | 36 | 48.36 | 7.8 | ||
| physical health-after 2 months | 36 | 52.58 | 10.84 | 0.002 | |
| physical health-after 2 months | 36 | 52.58 | 10.84 | ||
| physical health-after 6 months | 36 | 56.26 | 12.26 | 0.029 | |
| physical health-before | 36 | 39.2 | 6.67 | ||
| physical health-after 6 months | 36 | 56.26 | 12.26 | <0.001 | |
| Mediumrisk | physical health-before | 41 | 41.87 | 8.1 | |
| physical health-after 2 weeks | 41 | 48.88 | 10.61 | <0.001 | |
| physical health-after 2 weeks | 41 | 48.88 | 10.61 | ||
| physical health-after 2 months | 41 | 53.1 | 10.26 | 0.001 | |
| physical health-after 2 months | 41 | 53.1 | 10.26 | ||
| physical health-after 6 months | 41 | 56.13 | 12.42 | 0.019 | |
| physical health-before | 41 | 41.87 | 8.1 | ||
| physical health-after 6 months | 41 | 56.13 | 12.42 | <0.001 | |
| Highrisk | physical health-before | 3 | 53.33 | 6.88 | |
| physical health-after 2 weeks | 3 | 59.58 | 25.87 | 0.627 | |
| physical health-after 2 weeks | 3 | 59.58 | 25.87 | ||
| physical health-after 2 months | 3 | 60.41 | 24.07 | 0.944 | |
| physical health-after 2 months | 3 | 60.41 | 24.07 | ||
| physical health-after 6 months | 3 | 62.5 | 27.04 | 0.549 | |
| physical health-before | 3 | 53.33 | 6.88 | ||
| physical health-after 6 months | 3 | 62.5 | 27.04 | 0.547 | |
Table 4: Relationship between Orebro Musculoskeletal Pain Questionnaire (OMPQ) in patients in terms of mental health.
| Orebro Musculoskeletal PainQuestionnaire (OMPQ) | No. | Mean | Standard deviation |
P value. | |
|---|---|---|---|---|---|
| Low risk | mental health-before | 36 | 44.09 | 7.88 | |
| mental health-after 2 weeks | 36 | 45.95 | 6.42 | 0.197 | |
| mental health-after 2 weeks | 36 | 45.95 | 6.42 | ||
| mental health-after 2 months | 36 | 49.62 | 6.53 | 0.002 | |
| mental health-after 2 months | 36 | 49.62 | 6.53 | ||
| mental health-after 6 months | 36 | 53.26 | 8.25 | 0.007 | |
| mental health-before | 36 | 44.09 | 7.88 | ||
| mental health-after 6 months | 36 | 53.26 | 8.25 | <0.001 | |
| Medium risk | mental health-before | 41 | 45.16 | 7.84 | |
| mental health-after 2 weeks | 41 | 47.75 | 7.23 | 0.044 | |
| mental health-after 2 weeks | 41 | 47.75 | 7.23 | ||
| mental health-after 2 months | 41 | 50.23 | 7.73 | 0.042 | |
| mental health-after 2 months | 41 | 50.23 | 7.73 | ||
| mental health-after 6 months | 41 | 55.29 | 9.04 | 0.001 | |
| mental health-before | 41 | 45.16 | 7.84 | ||
| mental health-after 6 months | 41 | 55.29 | 9.04 | <0.001 | |
| High risk | mental health-before | 3 | 58.5 | 11 | |
| mental health-after 2 weeks | 3 | 67.87 | 16 | 0.147 | |
| mental health-after 2 weeks | 3 | 67.87 | 16 | ||
| mental health-after 2 months | 3 | 52.79 | 12.5 | 0.12 | |
| mental health-after 2 months | 3 | 52.79 | 12.5 | ||
| mental health-after 6 months | 3 | 52.3 | 7.56 | 0.891 | |
| mental health-before | 3 | 58.5 | 11 | ||
| mental health-after 6 months | 3 | 52.3 | 7.56 | 0.448 | |
Discussion
This study aimed to investigate the effect of preoperative anxiety and depression on the clinical consequences of discectomy in Rahnemoun Hospital from 2020 to 2022, which was conducted as a prospective study. According to the results, the Hospital Anxiety and Depression Scale (HDAS) questionnaire in the studied patients, based on the ODI questionnaire before surgery, two weeks, two months, and six months after surgery, show a significant difference. Moreover, the results of the Orebro Musculoskeletal Pain Questionnaire (OMPQ), in the studied patients, based on the ODI questionnaire, before surgery, two weeks, two months, and six months after surgery, did not show a significant difference.
In their study, evaluated the effect of depression, anxiety, and optimism on postoperative satisfaction and the clinical outcomes of patients with spinal stenosis and degenerative spondylolisthesis who underwent bilateral posterior fusion surgery. In this study, the VAS and ODI questionnaire scores were significantly reduced after surgery and indicated the desired outcomes, which is consistent with the results of the present study. There was no significant relationship between the patient's preoperative psychological status (anxiety, depression, and optimism) and improved postoperative clinical outcomes, measured using VAS and ODI, and are in line with our results. However, there was a significant relationship between postoperative satisfaction and optimism [40]. Conducted a study to evaluate preoperative anxiety on the consequences of two years after spinal surgery for pseudoarthrosis, Adjacent Segment Disease (ASD), and restenosis, similarly, as a prospective cohort study. According to the results, VAS score, two years after surgery, compared to before surgery, increased significantly in patients. Moreover, the DOI pain questionnaire score increased significantly in all three groups of patients. In addition, the increase of the
Preoperative Zhang Anxiety Scale significantly improved patients' disability in two future years. This study concluded that preoperative anxiety levels could be considered as predictors of functional outcomes after spinal surgery in patients with pseudoarthrosis, Adjacent Segment Disease (ASD), and restenosis at the same level. Conducted a cohort study entitled "Investigation of the relationship between preoperative psychological factors and poor outcomes in patients undergoing discectomy/laminectomy or spinal fusion. According to the results of this study, spinal surgery leads to a significant improvement in pain, functional ability, and medication. There is a significant relationship between psychological and drug use levels with poor outcomes. So, the results were poorer in patients with high risk, both psychologically and pharmacologically. In addition, the accuracy of PPS in predicting postoperative outcomes was 82%. Only 9 out of 53 patients with poor outcomes had low psychological and pharmacological risks [20]. In a prospective observational study, examined the effect of depressive symptoms on surgical outcomes among patients with spinal stenosis. The follow-up period of this study was five years. According to the results of this study, patients with a high rate of depression, compared to people with a low rate of depression, showed a higher ODI score in all follow-up stages. But there was no significant difference between the scores of the VAS questionnaire and depression. In the group with low depression, ODI scores and walking distance in the preoperative phase differed significantly from the 5-year follow-up. This difference was also observed in the group with high depression. The results show that long-term depression symptoms in LLS patients are related to an increased risk of poor functional ability after surgery [41]. Investigated the role of latent anxiety in persistent low back pain after lumbar disc surgery. A total of 108 patients with lumbar disc herniation participated in this study. According to the results of this study, before surgery, 72.2% of patients had overt anxiety, 54.6% had latent anxiety, and 11.1% had current depression. During the follow-up period, the prevalence of overt anxiety was significantly reduced, which was not consistent with the present study results. There was no change in the prevalence of latent anxiety, and a significant increase in the prevalence of current depression was observed. According to linear regression analysis, preoperative job anxiety was the primary determinant of postoperative pain. VAS scores were assessed by dividing patients into two groups based on their preoperative mental anxiety. The group affected by preoperative latent anxiety had significantly higher VAS scores in each follow-up period than patients with no preoperative latent anxiety [42].
In line with the results of this study and comparing it with other studies, it can be found that there are differences between the results of our study and some studies. Since depression and anxiety are multifactorial emotional disorders, examining a single surgical factor cannot explain depression and anxiety. Since different studies have been performed in different countries and regions, these differences may be due to differences in the study regions. Moreover, in different studies, the measuring instruments, including questionnaires and checklists, are different from each other, and each one used a different range scoring; therefore, another difference may be due to inconsistency in measuring instruments.
One of the study's limitations was data collection with a questionnaire, which was collected as a self-report from patients, because some patients may not have answered the questions honestly, which is very important to realize people's emotional and psychological problems.
Conclusion
According to the results of this study, it can be concluded that depression and anxiety, physical function, and other psychological variables of patients can improve after surgery. Future research is recommended using larger sample sizes at several centers.
References
- Maetzel A, Li L (2002) The economic burden of low back pain: a review of studies published between 1996 and 2001. Best Pract Res Clin Rheumatol 16:23-30
[Crossref] [Google Scholar] [Pubmed]
- Pai S, Sundaram LJ (2004) Low back pain: an economic assessment in the United States. Orthop Clin North Am 35:1-5
[Crossref] [Google Scholar] [Pubmed]
- Hoy D, Brooks P, Blyth F, Buchbinder R (2010) The epidemiology of low back pain. Best Pract Res Clin Rheumatol 24:769-781
[Crossref] [Google Scholar] [Pubmed]
- Weiner DK, Kim YS, Bonino P, Wang T (2006) Low back pain in older adults: are we utilizing healthcare resources wisely? Pain Med 7:143-150
[Crossref] [Google Scholar] [Pubmed]
- Hazard RG (2006) Failed back surgery syndrome: surgical and nonsurgical approaches. Clin Orthop Relat Res 443:228-32
[Crossref] [Google Scholar] [Pubmed]
- Aalto TJ, Malmivaara A, Kovacs F, Herno A, Alen M, et al. (2006) Preoperative predictors for postoperative clinical outcome in lumbar spinal stenosis: systematic review. Spine 31:648-663
[Crossref] [Google Scholar] [Pubmed]
- Den Boer JJ, Oostendorp RA, Beems T, Munneke M, Evers AW (2006) Continued disability and pain after lumbar disc surgery: the role of cognitive-behavioral factors. Pain 123:45-52
[Crossref] [Google Scholar] [Pubmed]
- Azizpoor Y, Hemmati F, Sayehmiri K (2013) Prevalence of life-time back pain in Iran: a systematic review and meta-analysis. BMC Nurs 18:102-112
[Crossref] [Google Scholar] [Pubmed]
- Jacobs WC, van Tulder M, Arts M, Rubinstein SM, van Middelkoop M, et al. (2011) Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review. Eur Spine J 20:513-522
[Crossref] [Google Scholar] [Pubmed]
- Azimi P, Mohammadi HR, Sadeghi S, Tabatabaiefar SM (2012) The predictive value of Japanese orthopaedic association score in patients diagnosed with lumbar disc herniation undergoing discectomy. Pajoohande 17:45-49
[Google Scholar] [Pubmed]
- Abrishamkar S, Kouchakzadeh M, Mirhosseini A, Tabesh H, Rezvani M, et al. (2015) Comparison of open surgical discectomy versus plasma-laser nucleoplasty in patients with single lumbar disc herniation. J Res Med Sci 20:1133
[Crossref] [Google Scholar] [Pubmed]
- Motiei-Langroudi R, Sadeghian H, Seddighi AS (2014) Clinical and magnetic resonance imaging factors which may predict the need for surgery in lumbar disc herniation. Asian Spine J 8:446-452
[Crossref] [Google Scholar] [Pubmed]
- Peul WC, Van Houwelingen HC, van den Hout WB, Brand R, Eekhof JA, et al. (2007) Surgery versus prolonged conservative treatment for sciatica. N Engl J Med 356:2245-2256
[Crossref] [Google Scholar] [Pubmed]
- Mashhadinezhad H, Ganjeifar B (2015) The correlation between the duration of sciatica and clinical outcome after lumbar discectomy. Ehran Univ Med J 73:176-181
[Google Scholar] [Pubmed]
- Katayama Y, Matsuyama Y, Yoshihara H, Sakai Y, Nakamura H, et al. (2006) Comparison of surgical outcomes between macro discectomy and micro discectomy for lumbar disc herniation: a prospective randomized study with surgery performed by the same spine surgeon. J Spinal Disord Tech 19:344-347
[Crossref] [Google Scholar] [Pubmed]
- Koes BW, Van Tulder M, Peul W (2007) Diagnosis and treatment of sciatica. Br Med J 334:1313
[Crossref] [Google Scholar] [Pubmed]
- Schoenfeld AJ, Weiner BK (2010) Treatment of lumbar disc herniation: evidence-based practice. Int J Gen Med 3:209-214
[Crossref] [Google Scholar] [Pubmed]
- Malter AD, Larson EB, Urban N, Deyo RA (1996) Cost-Effectiveness of Lumbar Discectomy for the Treatment of Herniated Intervertebral Disc. Spine 21:1048-1054
[Crossref] [Google Scholar] [Pubmed]
- Williamson E, White L, Rushton A (2007) A survey of post-operative management for patients following first time lumbar discectomy. Eur Spine J 16:795-802
[Crossref] [Google Scholar] [Pubmed]
- Block AR, Ohnmeiss DD, Guyer RD, Rashbaum RF, Hochschuler SH (2001) The use of presurgical psychological screening to predict the outcome of spine surgery. Spine J 1:274-282
[Crossref] [Google Scholar] [Pubmed]
- Adogwa O, Parker SL, Shau DN, Mendenhall SK, Aaronson OS, et al. (2012) Preoperative zung depression scale predicts outcome after revision lumbar surgery for adjacent segment disease, recurrent stenosis, and pseudarthrosis. Spine J 12:179-185
[Crossref] [Google Scholar] [Pubmed]
- Daubs MD, Norvell DC, McGuire R, Molinari R, Hermsmeyer JT, et al. (2011) Fusion versus nonoperative care for chronic low back pain: do psychological factors affect outcomes. Spine 36:96-109
[Crossref] [Google Scholar] [Pubmed]
- Lee JS, Park YM, Ha KY, Cho SW, Bak GH, et al. (2016) Preoperative anxiety about spinal surgery under general anesthesia. Eur Spine J 25:698-707
[Crossref] [Google Scholar] [Pubmed]
- Ghanei RG, Rezaei K, Mahmoodi R (2013) The relationship between preoperative anxiety and postoperative pain after cesarean section. Iran J Obstet Gynecol Infertil 15:16-22
[Crossref] [Google Scholar] [Pubmed]
- Ganji T, Hosseini A (2011) Under graduate nursing students' religious beliefs and their relationship with anxiety. Iran J Nurs Res 23:44-51
- Nazari-Vanani R, Rahimi-Madiseh M, Drees F (2014) Evaluation of preoperative anxiety and stress, and ways to modify it, the patients in Kashani hospital operating room in 2013. J Clin Nurs 2:53-60
[Pubmed]
- Momeni K, Karimi H (2011) Comparison of mental health between elderly admitted in sanitarium with elderly in sited in personal home. J Kerman Univ Med Sci 14:79446
- Matthias AT, Samarasekera DN (2012) Preoperative anxiety in surgical patients-experience of a single unit. Acta Anaesthesiol Taiwan 50:3-6
[Crossref] [Google Scholar] [Pubmed]
- Roohy GR, Rahmany A, Abdollahy AA, Mahmoody GHR (2005) The effect of music on anxiety level of patients and some of physiological responses before abdominal surgery. J Babol Univ Med Sci 7:75-78
[Google Scholar] [Pubmed]
- Cooke M, Chaboyer W, Hiratos MA (2005) Music and its effect on anxiety in short waiting periods: a critical appraisal. J Clin Nurs 14:145-155
[Crossref] [Google Scholar] [Pubmed]
- Bringuier S, Dadure C, Raux O, Dubois A, Picot MC, et al. (2009) The perioperative validity of the visual analog anxiety scale in children: a discriminant and useful instrument in routine clinical practice to optimize postoperative pain management. Anesth Analg 109:737-744
[Crossref] [Google Scholar] [Pubmed]
- De Groot KI, Boeke S, van den Berge HJ, Duivenvoorden HJ, Bonke B, et al. (1997) The influence of psychological variables on postoperative anxiety and physical complaints in patients undergoing lumbar surgery. Pain 69:19-25
[Crossref] [Google Scholar] [Pubmed]
- Hickey OT, Burke SM, Hafeez P, Mudrakouski AL, Hayes ID, et al. (2010) Determinants of outcome for patients undergoing lumbar discectomy: a pilot study. Eur J Anaesthesiol 27:696-701
[Crossref] [Google Scholar] [Pubmed]
- Schillberg B, Nyström B (2000) Quality of life before and after microsurgical decompression in lumbar spinal stenosis. J Spinal Disord 13:237-241
[Crossref] [Google Scholar] [Pubmed]
- Trief PM, Grant W, Fredrickson B (2000) A prospective study of psychological predictors of lumbar surgery outcome. Spine 25:2616-2621
[Crossref] [Google Scholar] [Pubmed]
- Trief PM, Ploutz-Snyder R, Fredrickson BE (2006) Emotional health predicts pain and function after fusion: a prospective multicenter study. Spine 31:823-830
[Crossref] [Google Scholar] [Pubmed]
- Junge A, Dvorak J, Ahrens S (1995) Predictors of bad and good outcomes of lumbar disc surgery. Spine 20:460-468
[Crossref] [Google Scholar] [Pubmed]
- Junge A, Fröhlich M, Ahrens S, Hasenbring M, Sandler AJ, et al. (1996) Predictors of bad and good outcome of lumbar spine surgery: a prospective clinical study with 2 years' follow-up. Spine 21:1056-1064
[Crossref] [Google Scholar] [Pubmed]
- Arpino L, Iavarone A, Parlato C, Moraci A (2004) Prognostic role of depression after lumbar disc surgery. Neurol Sci 25:145-147
[Crossref] [Google Scholar] [Pubmed]
- Lee J, Kim HS, Shim KD, Park YS (2017) The effect of anxiety, depression, and optimism on postoperative satisfaction and clinical outcomes in lumbar spinal stenosis and degenerative spondylolisthesis patients: cohort study. Clin Orthop Surg 9:177-183
[Crossref] [Google Scholar] [Pubmed]
- Pakarinen M, Vanhanen S, Sinikallio S, Aalto T, Lehto SM, et al. (2014) Depressive burden is associated with a poorer surgical outcome among lumbar spinal stenosis patients: a 5-year follow-up study. Spine J 14:2392-2396
[Crossref] [Google Scholar] [Pubmed]
- D'angelo C, Mirijello A, Ferrulli A, Leggio L, Berardi A, et al. (2010) Role of trait anxiety in persistent radicular pain after surgery for lumbar disc herniation: a 1-year longitudinal study. Neurosurg 67:265-271
[Crossref] [Google Scholar] Pubmed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences