The Utility of Thulium Laser in Neuroendoscopy
Oppido PA and Cattani F
DOI10.21767/2471-9633.100015
Oppido PA* and Cattani F
Neurosurgery, National Cancer Institute Regina Elena, Rome, Italy
- *Corresponding Author:
- Piero Andrea Oppido
MD, PhD, Neurosurgery
National Cancer Institute, Rome, Italy
Tel: 0652666757
E-mail: oppido@ifo.it
Received: April 08, 2016; Accepted: May 24, 2016; Published: May 31, 2016
Citation: Oppido PA, Cattani F. The Utility of Thulium Laser in Neuroendoscopy. Neurosurg. 2016, 1:2.
Abstract
In the last years, neuroendoscopy has gained consensus as a minimally invasive surgical approach to ventricular lesions. The magnification of the endoscope has become wonderful, but the bleeding control and tumor ablation continue to be harmful by standard tools only through the working channel. Specially, in vascularized tumors and near vital structures the traditional electrosurgery can be ineffective and dangerous. Since 2009, we are using the Tu diode pumped solid state (DPSS) laser (Revolix, LISA laser products) to improve neuroendoscopic procedures. In the Tu DPSS laser the active material is thulium (Tu), emitting light at wavelength of 2,0 μ, through one microfiber large 0,2 mm in diameter introduced in the endoscope working channel. The Tu DPSS laser works very well in water solution, as in the CSF of the ventricles. This laser can hit the tumor by touching or targeting from short distance with low penetration. Tumor cutting and ablation is possible, too. We report our experience in 26 ventricular tumors, 16 in 3rd ventricle and 10 in the lateral ventricle. The histology was: 13 high grade glioma, 5 craniopharyngiomas, 2 PNET, 2 metastasis, 4 colloid cysts. A flexible or rigid scope was used. In 18 neuroendoscopic biopsies the Tu DPSS laser microfiber was used for hemostasis and partial ablation. In 5 craniopharyngiomas wall ablation was performed. In 4 colloid cysts complete removal was possible in one case 3rd ventricular nodule was totally removed by Tu laser ablation. The ETV or tumors cyst fenestration or septostomy through infiltrated septum was successfully performed. The Tu laser showed precise coagulation at low temperature without tissue sticking. In all surgical procedures bleeding control was easy and successful. During Tu laser activation endoscopic vision was always clear. No side effects due to this device were observed. We consider Tu DPSS laser extremely handle and safe. The Tu laser is very efficient for coagulation and ablation of vascularized tumors.
Keywords
Neuroendoscopy; Thulium; Laser; Coagulation; Ablation; Microsurgery
Introduction
Neuroendoscopy is presently considered a minimally invasive surgical approach. Comparatively, a microsurgical approach to ventricles allows using quickly several instruments and material for hemostasis, cutting and excision. Despite wonderful magnification recently improved, the bleeding control and tumor ablation are harmful by standard tools through the narrow channel of the neuroendoscope. Specially, in vascularized tumors and near vital structures the traditional electrosurgery can be ineffective and dangerous. In ventricular neuroendoscopy the ideal tool is one thin instrument for easy coagulation, cutting and ablation by saving healthy tissue. Laser is the instrument that can realize these effects through one working channel without changing several devices and time consuming. Since the 1960s many types of lasers have been used in neurosurgery [1]. In literature, the most popular lasers used in neurosurgery consist of different medium (CO2 or Nd: YAG) with different properties, based on: wavelength (micron, μ), power output (watts), beam density (spot size) and time of exposure. The CO2 laser is an excellent cutting tool, but has a limited hemostasis control. The Nd: YAG laser is very useful for coagulation, but has wide thermal effects. Both lasers work only in air and not in aqueous field as in the cerebral spinal fluid (CSF) of ventricles. Since 2007, the thulium (Tu) laser (Revolix Jr., LISA laser products) has been introduced in neuroendoscopy for third ventriculostomy (ETV) [2]. It can work in air or water solutions with the same result like in urology. For these properties, since 2009 we chose the Tu laser in our neuroendoscopic procedures for ventricular tumors.
Methods
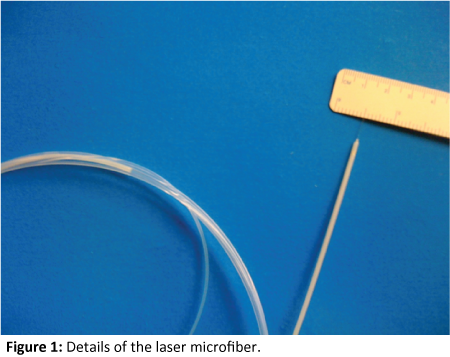
Tu laser properties: it is a diode pumped solid state (DPSS) laser. In the Tu DPSS the active laser material is thulium (Tu), emitting light at wavelength of 2.0 μm, through one optic microfiber large from 0,2 mm to 1 mm in diameter (Figure 1). The laser microfiber is flexible and so long enough that can be used in steerable flexible endoscope. Its wavelength is selectively absorbed by water and can be conveyed by thin microfibers (0.2–1.0 mm) through the endoscope’s working channel (>1,2 mm). The Tu DPSS laser can work in air space like in assisted endoscopy or microsurgery, but in our hands was used inside water solution, as the CSF, for ventricular neuroendoscopy. The power output range is from 0.5 W to 15 W. In the CSF the laser energy is absorbed by the water that reduces thermal effects. It can be used in continuous or pulse mode by using focused beam, identified as a red spot over the tissue surface. By the tip of the laser microfiber it’s possible to hit the tumor by touching or targeting from short distance with limited tissue penetration (<1 mm), as histologically tested. Both tumor cutting or photocoagulation or photovaporization are possible. Continuous endoscopic rinsing ensures the normal temperature in the ventricles.
Personal experience from 2009 to 2015 in 26 neuroendoscopic procedures for ventricular tumors by flexible or rigid scope the Tu laser was applied. The microfiber diameter was about 0.2 mm. Patient's age ranged from 16 to 75 years. The site was in 16 tumors the 3rd ventricle and in 10 the lateral ventricle. At MRI 20 tumors showed contrast enhancement. Histology was: 13 high grade glioma, 5 craniopharyngiomas, 2 PNET, 2 metastasis and 4 colloid cysts.
Results
In 18 neuroendoscopic biopsies the Tu DPSS laser microfiber was used for cutting and hemostasis of much vascularized tumors (Figure 2). In 4 tumors partial resection was achieved. In 5 craniopharingiomas by laser ablation cystic wall was totally removed. In 2 of them the solid calcified nodule was reduced.
In 8 cases the septostomy through an infiltrated or thick septum was successfully performed. In 10 cases the ETV was associated. All 4 colloid cysts were totally removed by Tu laser, after choroid plexus coagulation. The power output ranged from 1 W to 8 W: it was below (1 W–4 W) in soft tissue, higher (5 W–8 W) in hard and bleeding tissue. It showed precise coagulation at low temperature without tissue sticking. In all surgical procedures bleeding control was easy and successful. In all procedures the precise cutting and shrinking was without any surgical stress on the surrounding anatomical structures. The limits of laser necrosis in the tumor specimen were visible, histologically. No thermal damage or other complications due to the Tu laser were registered. During laser activation endoscopic vision was always clear without air bubbles.
Discussion
Since the early 1960s, CO2, NdYAG and other laser prototypes have been widely used in neurosurgery [1]. By the laser wavelength is determined the energy absorption in tissue and water with rapid conversion of light energy into heat in a small volume of tissue. The laser has the property to cut tumor or photocoagulation or photovaporization with only one instrument: this concept is essential in neuroendoscopic procedures for ventricular tumors. In fact, in rigid or flexible ventricular endoscope there is only one working channel and the change of instruments is time consuming or harmful, especially in case of important bleeding. The most common in neurosurgery is the CO2, but it works only in air medium. The Tu laser was initially used in urological surgery because it can work in aqueous medium and later in micro-neurosurgery for brain tumors along narrow corridors [3]. In our experience, the use of Tu laser in microsurgery or in assisted endoscopy was a skill learning curve. In 2007 the first experience in neuroendoscopy to perform ETV was reported [2]. The Tu laser efficacy both in coagulation both in tissue ablation makes itself an elective tool in neuroendoscopy, especially for ventricular tumors. Because of tumor bleeding, neuroendoscopic biopsy is generally limited to not-vascularized tumors, but in our experience we were able to treat vascularized tumors (Figure 2), too. The precise cutting allows the tumor resection close to vital structures, without injury and limited penetration or diffusion. In selected cases the tumor debulking was possible and the vaporization of soft tissue quick and easy. The Tu laser’s wavelength is close to the absorption band of water (1.92 nm); therefore, thermal damage is ineffective. The laser microfiber is flexible and handles to work, so much to be introduced in steerable flexible endoscope. This capacity was excellent to work in the posterior part of 3rd ventricle. Furthermore, the Tu laser makes easy any kind of septostomy, getting wide corridors through tick and infiltrated septum pellucidum as in ventricular tumors, too. The combination of precise cutting and coagulation helped in colloid cyst removal, after choroid plexus shrinking. In this series no hemorrhage or other complications were registered, meaning the safety of this laser. Recently, in neuroendoscopy a new ultrasonic aspirator has been introduced [4]. Despite laser, in this case only changing instruments in the working channel the hemostasis is possible. Actually, in ventricular tumors neuroendoscopy the laser represents the only instrument getting simultaneous bleeding control, precise cutting and tissue ablation without time consuming and several passages through the endoscopic working channel.
Conclusion
Despite the innovation technology in neuroendoscopy, bleeding control and tumor ablation are yet harmful and time consuming. The Tu laser is an efficient energy source that can be transported through very thin flexible fibers, across one endoscopic working channel. Furthermore, for its property to work in aqueous solution it is very efficient for coagulation and ablation of vascularized ventricular tumors, by preserving healthy tissue. Comparing with ultrasonic aspirator, it is no necessary change instrument for hemostasis. The present results show that the Tu laser is extremely handy and safe as a reliable dissecting method for neuroendoscopic procedures.
Recommendation
We recommend learning the laser characteristics in microsurgery. After a short learning curve, the Tu laser can be used in ventricular neuroendoscopy. We suggest starting using low watt energy and increase the power for bleeding or hard tissue.
References
- Ryan RW, Spetzler RF, Preul MC (2009) Aura of technology and the cutting edge: A history of lasers in neurosurgery. Neurosurg Focus 27: E6.
- Ludwig HC, Kruschat T, Knobloch T, Teichmann HO, Rostasy K, et al. (2007) First experience with a 2.0 micron near infrared laser system for neuroendoscopy. Neurosurg Rev 30: 195-201.
- Passacantilli E, Antonelli M, D'Amico A, Delfinis CP, Anichini G, et al. (2012) Neurosurgical applicationsof the 2 µm thulium laser: Histological evaluation of meningiomas in comparison to bipolar forceps and ultrasonic aspirator. Photomed Laser Surg 30: 286-292.
- Oertel J, Krauss JK, Gaab MR (2008) Ultrasonic aspiration in neuroendoscopy: First results with a new tool. J Neurosurg 109: 908-911.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences