Gamma Knifeî Radiosurgery for Trigeminal Neuralgia
Alexandra Lyons*1, Mark Pinkham2, Matthew Foote3, Sarah Olson4, Heath Foley5, Bruce Hall6
1Department of Neurosurgery registrar, MBBS, MMed, Australia
2Department of Radiation Oncologist, BM, BCh MA (Hons), FRANZCR, Australia
3Department of Radiation Oncologist, MBBS (Hons), BSc, FRANZCR, Australia
4Department of Neurosurgeon, MBBS, MBChB, MPhil, FRACS, Australia
5Department of Radiation therapist, BAppSc (MRT), Australia
6Department of Director of Neurosurgery, MBBS, FRACS, CIME, Australia
- *Corresponding Author:
- Alexandra Lyons
Department of Neurosurgery registrar, MBBS, MMed, Australia
Tel No: 0455991456
E-mail: arlyons05@gmail.com
Received Date: August 13, 2021; Accepted Date: November 16, 2021; Published Date: November 26, 2021
Citation: Lyons A, Pinkham M, Foote M, Olson S, Foley H, Hall B (2021) Gamma Knife® Radiosurgery for Trigeminal Neuralgia, Neurosurg, Vol:5 No: 5 .
Abstract
Background
Trigeminal neuralgia (TN) affects up to 0.3% of the population with pain often difficult to manage. It commonly affects patients over 50 years, and occurs more frequently in women. Treatment options include medical therapy, surgery (microvascular decompression (MVD) and percutaneous balloon compression (PBC)) and Gamma Knife® radiosurgery (GKRS). GKRS has been available at the Princess Alexandra Hospital since October 2015. Our objective was to evaluate the efficacy of GKRS on patients with TN and investigate the impact of known prognostic variables on patient outcomes.
Method
A retrospective review was conducted on all patients who received GKRS for TN from October 2015 till March 2018 in a single center tertiary neurosurgical referral hospital.
Results
43 patients with TN were treated with GKRS with a median follow up time after treatment of 7 months (6 weeks - 36 months). Median age was 69 years, 51% were female and 21% had atypical symptoms. 33% had previously had surgery (7=MVD, 7=PBC). Clinical benefit after GKRS was observed in 79% of patients at 1 month, 73% at 3 months, 74% at 6 months and 87% at 1 year. Of the 49% who experienced a relapse of pain within 1 year post GKRS, the median time to relapse was 8 weeks. No serious adverse events or severe toxicity were recorded. Patient and treatment factors that predicted worse outcomes were the presence of a vessel contacting the nerve, female gender and a higher radiation dose.
Conclusion
GKRS is an effective treatment option for patients with TN and it is particularly useful to consider in those with co-morbidities that make surgery high risk. GKRS has acceptable short-term beneficial results in TN, however with relapse other treatment options may be required.
Introduction
Trigeminal Neuralgia (TN) is a chronic neuropathic pain condition which is characterized by paroxysmal, lancinating, electric shock like pain in one or more divisions of the trigeminal nerve. It affects up to 0.3% of the population, predominantly female patients over the age of 50, and the pain is often difficult to manage [1]. Treatment options include medical therapy, surgery (microvascular decompression (MVD), radiofrequency ablation (RA), percutaneous balloon compression (PBC), glycerol rhizotomy (GR)) and Gamma Knife® radiosurgery (GKRS).
Gamma Knife® works by using 3 dimensional coordinates incorporated into the Leksell frame which is screwed into the periosteum of the patient’s skull. The co-ordinates on MRI are integrated with the Gamma Knife® software to triangulate the exact spatial location of the chosen treatment area in relation to the frame. The patient, with frame attached, is then secured to the machine so that no movement can occur to ensure millimeter accuracy. The target is placed at the center of the converging Cobalt-60 gamma radiation beams and the prescribed treatment dose is delivered.
The aim of this review is to contribute data on GKRS from a contemporary Australian series. The Princess Alexandra Hospital is the only hospital in Australia to provide GKRS to the public sector with no out-of-pocket expenses. MVD is considered gold standard if there is a vessel identified compressing the trigeminal nerve [2], and has been shown to improve patients’ quality-adjusted life years by 8.2, compared to 4.9 with GKRS [3]. GKRS is thought to be a good second line therapy for TN and is commonly performed when patient choice and co-morbidities preclude the use of MVD. Other therapies such as PBC, GR and RA all provide good initial analgesia (~80%), however side effects are more prevalent than GKRS, and GR in particular has a high short-term recurrence rate [4,5].
Factors which are more likely to result in recurrence of pain in GKRS for TN are increased age, atypical symptoms, prior surgery and multiple divisions of the trigeminal nerve affected [6]. Serious complications of GKRS are rare, the main complication is a 14% chance of facial numbness [7]. Patients who develop facial numbness have better long-term pain control [8, 9].
Methods
A single center retrospective review was undertaken for all patients who received GKRS for TN at the Princess Alexandra Hospital in Australia from October 2015 till March 2018. No exclusion criteria were present. Patients were followed up till March 2020, with a median follow up time of 12 months (3 months - 3 years).
A Leksell frame was placed on each patient under local anaesthetic, after which an MRI was obtained. Treatment planning was undertaken by a radiation oncologist and medical physicist, with collaboration from a neurosurgeon. The nerve root entry zone of the trigeminal nerve was the target isocentre for radiation. The patient with frame attached was then secured to the Gamma Knife® machine for treatment. The frame was removed post treatment and patients were discharged after an observation period.
Patients received a phone call day 1 post procedure by the GKRS nurse and were followed up at 1 month, 3 months, 6 months (+/- ongoing) where pain, medication requirement and complications were assessed. If a patient had an excellent result at the 3 month follow-up, they were often discharged from clinic and only seen again if relapse of symptoms occurred - either through GP referral or self referral via phoning the clinic. Pain levels and medication requirement were assessed against the Barrow Neurological Institute (BNI) pain intensity scoring system (Table 1). Demographics and treatment information were obtained from medical records.
Independent statistical analysis was obtained with descriptive statistics using mean and standard deviation for continuous data normally distributed or median and inter-quartile range when normality was not met. Normality was assessed using the Shapiro-Wilk test.
| Pain score (Class) | Definition |
|---|---|
| l | No pain and taking no medication |
| II | Occasional pain, but 1aking nomedica1ion |
| Ill | |
| A | No pain, but taking medication |
| B | Pain presen1, bu1adequatelycontrolled with |
| IV | Pain improved, but not adequa1clycon1rolled |
| v | No relief |
Table 1:Barrow Neurological Institute (BNI) pain intensity score
Results
Patient demographics
Of the 43 patients, there was a slight female preponderance, and a median age of 69 years (46-88 years). 9 patients had atypical symptomatology, 3 had bilateral symptoms and 14% had a secondary aetiology causing trigeminal neuralgia. V2 (70%) and V3 (60%) were the most affected branches of the trigeminal nerve. 18 patients had previous failed treatments before having GKRS, of those 7 had an MVD and 7 had PBC. See Table 2.
20 patients had a vessel identified compressing the trigeminal nerve on fine cut reconstructed T2 MRI of the posterior fossa, with the superior cerebellar artery being the most common. See Table 3. The average width of the compressive vessel was 1.3mm. Two patients had vascular malformations causing compression of the trigeminal nerve.
| n | % | ||
| Age | =/>70 years | 23 | 53 |
| <70 years | 20 | 47 | |
| Gender | Male | 20 | 47 |
| Female | 23 | 53 | |
| Symptoms | Typical | 35 | 79 |
| Atypical | 8 | 21 | |
| Aetiology | primary | 37 | 86 |
| Secondary | 6 | 14 | |
| Side Affected | unilateral | 40 | 14 |
| bilateral | 3 | 93 | |
| Branch Affected | VI | 15 | 35 |
| V2 | 30 | 70 | |
| V3 | 26 | 60 | |
| Previous treatments | MVD | 7 | 16 |
| Balloon compression | 7 | 16 | |
| Nerveorganglion block | 5 | 12 | |
| Botox | 3 | 7 | |
| RFA | 1 | 2 | |
| Medicationonly | 27 | 63 | |
| Single previous treatment | 9 | 21 | |
| Multiple Previous treatments | 9 | 21 | |
| Years of diagnosis to GKRS | |||
| < lOyears | 27 | 63 | |
| >!O years | 16 | 37 |
Table 2:Relationship between pain score at 12 months and potential
| n | % | |
| No vessel identified | 23 | 53 |
| vessel identified | 20 | 47 |
| SCA | 13 | |
| AICA | 2 | |
| PICA | 1 | |
| Vein | 2 | |
| AVM | 2 |
Table 3: Trigeminal nervecompression
Radiosurgery dosage
14 patients received 80 Gray @ 100% isodose to the trigeminal nerve root entry zone and 29 patients received an 85 Gray dose. The median dose rate effect was 2.884 (2.582 - 3.54) and the average distance from the isocentre of radiation to the brainstem was 3.6mm (2.1 – 5.7mm).
1 patient was treated with GKRS a second time. She had recurring classical unilateral V3 distribution TN, had previously had an MVD followed by an excellent response to initial GKRS for 2 years. Her first treatment was with 80 Gray with a 3.3mm isocenter, and the second treatment 2.5 years later was 75 Gray with a 7.5mm isocenter distance from the brainstem.
Pain analysis
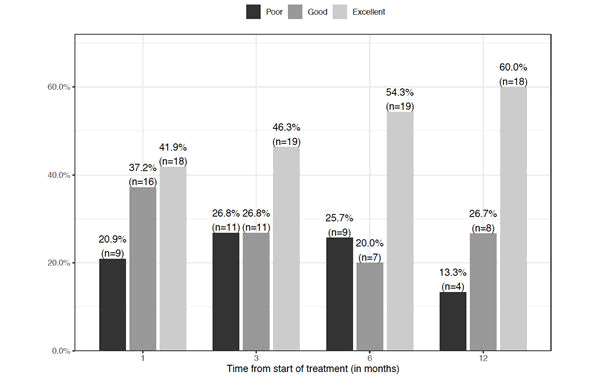
An excellent result is classified as a BNI pain score of 1 and 3a (no pain), good result as a BNI pain score of 2 and 3b, and a poor result with a score of 4 or 5, refer to Table 1. 79% of patients noticed immediate benefit within 1 day of treatment. An excellent result occurred in 42% of patients at 1 month, 46% at 3 months, 54% at 6 months and 60% at 1 year. An overall beneficial result (excellent or good) from GKRS occurred in 79% at 1 month, 73% at 3 months, 74% at 6 months and 87% at 1 year. The results at 1 year do not include 8 patients lost to follow up because they were previously discharged due to an excellent result. The majority of patients were lost to follow up after 1 year.
The median time to pain relief was 1 day and the median time to relapse was 8 weeks in patients who had acute flare ups. 14 patients required salvage treatment: 3 had MVD, 3 had PBC, 1 had repeat GKRS, 2 required significant analgesics such as ketamine and 4 required an increased dosage of medication or new agent to control the recurrence. 2 of the 4 patients with a poor pain result at the 1 year period ended up with an excellent outcome after receiving salvage treatment, while the other 2 had ongoing pain despite salvage attempts.
A sub group analysis was performed investigating patient characteristics affecting outcome. Patients who received 80Gy had more excellent results and fewer poor results consistently over all time periods (p value 0.08 at 1 month). At 12 months 70% of patients who didn’t have a vessel contacting the trigeminal nerve had excellent results, compared to only 1 patient with no vessel who had a poor result. Vessel contact was the most significant factor in patients who improved pain scores from 1 month to 12 months (p value 0.06). Males fared better than females. Interestingly there was no statistical difference between typical and atypical symptomatology and primary and secondary aetiology of TN on pain outcomes. There was no correlation between patients who had prior treatment and those that required salvage treatment after GKRS. Not surprisingly, if patients required rescue salvage treatment after GKRS, they were more likely to have an unfavourable outcome (p value 0.01).
| Variable | Excellent | Good | Poor | P-value |
|---|---|---|---|---|
| Vessel_cat | 0.33 | |||
| No | 12 (70.593%) | 4 (23.533%) | 1 (5.883%) | |
| Yes | 6 (46.153%) | 4 (30.773%) | 3 (23.083%) | |
| Complicat ions_cat | 0.57 | |||
| No | 10 (55.563%) | 6 (33.333%) | 2(11.113%) | |
| Yes | 8 (66.673%) | 2 (16.673%) | 2 (16.673%) | |
| Classical.vs.atypical.symptoms | 0.82 | |||
| atypical | 4 (803%) | 1 (203%) | 0 (03%) | |
| classical | 14 (563%) | 7 (283%) | 4 (16%) | |
| Gender | 0.66 | |||
| F | 9 (52.943%) | 5 (29.413%) | 3 (17.653%) | |
| M | 9 (69.233%) | 3 (23.083%) | 1 (7.693%) | |
| Primary.vs.secondary_cat | 0.64 | |||
| 1 | 15 (603%) | 6 (243%) | 4 (16%) | |
| 2 | 3 (603%) | 2 (403%) | 0 (03%) | |
| Dose.of.XRT | 0.86 | |||
| 80Gy | 7 (703%) | 2 (203%) | 1 (10%) | |
| 85Gy | 11 (553%) | 6 (303%) | 3 (15%) | |
| Age_cat | 0.52 | |||
| <70 | 9 (603%) | 5 (33.333%) | 1 (6.673%) | |
| >=70 | 9 (603%) | 3 (203%) | 3 (20%) | |
| Branch .affected cat | 1 | |||
| Multiple | 9 (603%) | 4 (26.673%) | 2(13.333%) | |
| Single | 9 (603%) | 4 (26.673%) | 2(13.333%) | |
| Branch .affected Vl | 0.66 | |||
| Vl-NOT-involved | 12 (63.163%) | 4 (21.053%) | 3 (15.793%) | |
| Vlinvolved | 6 (54.553%) | 4 (36.363%) | 1 (9.093%) | |
| Branch .affected V2 | 0.62 | |||
| V2involved | 12 (57.143%) | 5 (23.813%) | 4 (19.053%) | |
| V2-NOT-involved Branch .affected V3 | 6 (66.673%) | 3 (33.333%) | 0 (03%) | 0.59 |
| V3involved | 10 (62.53%) | 5 (31.253%) | 1 (6.253%) | |
| V3-NOT-involved | 8 (57.143%) | 3 (21.433%) | 3 (21.433%) | |
| time.to.pain.relief_cat | 0.54 | |||
| < ld | 13 (54.173%) | 7 (29.173%) | 4 (16.673%) | |
| >=ld | 5 (83.333%) | 1 (16.673%) | 0 (03%) | |
| Prev.Txcat | 0.59 | |||
| No | 10 (62.53%) | 3 (18.753%) | 3 (18.753%) | |
| Yes | 8 (57.143%) | 5 (35.713%) | 1 (7.143%) | |
| Salvage.treatments_cat | 0.01 |
Table 4: Relationship between pain score at 12 months and potential
Interestingly 1 patient with secondary TN due to demyelinating neuropathy had an excellent delayed response. Within the first 4 months post GKRS he received salvage treatment with ketamine cream, lignocaine patch and botox with no relief from his symptoms at 6 month follow up. No other salvage treatment was done and at the 1 and 2 year review, he was completely pain free off medications which could only be explained by a delayed analgesic response from GKRS.
Complications
There was no severe toxicity recorded. 11 patients experienced facial numbness or paresthesia following GKRS, 7 of which received 85Gy. 1 patient developed delayed analgesia dolorosa 1 year post GKRS (85Gy dosing). 1 patient felt mild nausea, 1 had vertigo, 1 suffered persisting unilateral hearing loss. 1 patient had temporary facial nerve weakness and 1 patient developed bothersome tongue numbness which resolved and an associated loss of taste. 1 patient had a pin site infection from the frame. Overall the majority of complications were minor with facial numbness being inconvenient but not concerning for most patients. There was no difference in developing numbness between treatment naïve patients compared to those with prior treatment. Bothersome complications were predominantly temporary. 65% of patients did not experience any complication. There was no statistically significant correlation between complications and isocenter distance (millimeters) from the brainstem in this cohort of patients.
| 80Gy | 85Gy | |
|---|---|---|
| No_complication | 9 | 19 |
| Numbers | 4 | 7 |
| Other_complication | 1 | 2 |
Table 5:Numbness complication vs dose
| Complication group | n | mean | sd | min | Q1 | median | Q3 | max |
|---|---|---|---|---|---|---|---|---|
| No_complication | 28 | 3.49 | 0.83 | 1.7 | 3.15 | 3.55 | 3.92 | 5.7 |
| Numbness | 11 | 3.69 | 1.11 | 2.4 | 3.05 | 3.3 | 4.3 | 6 |
| Other_complication | 3 | 3.8 | 0.46 | 3.3 | 3.6 | 3.9 | 4.05 | 4.2 |
Table 6: Description of isocentre to brainstem by complication group
Discussion
GKRS is postulated to work by iatrogenically inducing focal axonal degeneration of the sensory root of the trigeminal nerve, where pain fibers are more sensitive to injury than sensory fibres [8,10]. Irradiated trigeminal nerves of baboons and postulated that acute radiation-induced inflammatory changes are responsible for impaired pain transmission and consequent analgesia encountered within 48 hours [11]. This coincides with the 2 major peaks of time to analgesia following GKRS being described as within 48 hours and at 30 days [12]. Histologically the principle effect is primary axonal injury, which is dose related, with neuronal necrosis occurring at 100 Gray [11].
Studies investigating GKRS in TN primarily examine classical TN exclusively. Major international prospective and retrospective studies (with a combined cohort of 1168 patients) found on average 90% of patients had analgesia within a month, with 70% of patients remaining pain free at 1 year [12-14]. At 5 years, patients were pain free without medication in 61% of MVD cases and 47% of GKRS [14]. Interestingly we found patients improved over time, with 42% being pain free at 1 month, and 60% pain free at 1 year (72% if including patients discharged prior to 1 year given excellent results), despite including patients with secondary TN and atypical symptomatology who were predicted to have poorer outcomes.
Factors associated with poorer outcomes in our study were the presence of a vessel contacting the nerve, females and higher radiation dose (85Gy). Observed the best predictors for success in GKRS was a single branch affected, typical symptomatology and 1 failed procedure (compared to many) [9]. Historically there has been progressively less benefit with each successive treatment for resistant TN [15]. The development of facial paresthesia has been linked with longer term pain relief [8-10,12,14], however delayed presentations of anaesthesia dolorosa have been described with GKRS [16]. Motor dysfunction is often temporary [16].
The recurrence time of 8 weeks observed in our study is fitting with the biphasic response not uncommonly seen with GKRS for TN. This is much shorter than what has been found in other studies with a median time to recurrence ranging from 6 months to 6 years [6,7,9,12,17]; which perhaps reflects our inclusion of transient recurrences, hence potentially over-estimating the recurrence rate.
The single patient who received a second Gamma Knife® treatment had no relief/ minimally worse symptoms 2 months post repeated treatment. This is following an excellent response lasting 2 years from her first treatment. Other studies have found on average 88% of re-treated GKRS patients get a good result with >50% pain relief [18,19]. There has been no correlation found when predicting outcome success between the interval of first and second treatments, however most studies recommend a minimum wait period of 1 year [19]. Repeat GKRS however comes at the cost of a significantly higher risk of causing new facial numbness, which can be bothersome to patients [19]. Predictors for a successful repeat treatment of GKRS are a good initial response and numbness associated with the first GKRS treatment [20]. Negative predicators include failed response to first treatment and prior surgical procedures [19].
In regard to radiotherapy considerations, dose rate has not been associated with complications [8]. 1 vs 2 isocenters was trialed in a prospective study to see if nerve length irradiated made a difference. It was associated with increased numbness and made no difference to pain relief [21]. The risk of facial numbness increases with the dose of radiotherapy, with doses of 90 Gray having up to a 50% chance of causing facial nerve dysfunction [22].
Conclusion
Gamma Knife® Radiosurgery is an effective second line therapy in the management of trigeminal neuralgia. When age or co-morbidities preclude safe operating conditions for a microvascular decompression, GKRS treatment should be considered. 87% of patients in our study had clinically beneficial results (good or excellent) at one year with minimal complications.
References
- De Toledo IP, Reus JC, Fernandes M, Porporatti AL, PeresMA et al. (2016) Prevalence of trigeminal neuralgia: a systematic review. J AmDent Assoc 147:570-576.
- Burchiel K(2016) Trigeminal neuralgia: new evidence for origins and surgical treatment.Neurosurgery 63 Suppl 1:i52-55.
- Sivakanthan S, Van Gompel JJ, Alikhani P, Van Loveren H,Chen R et al. (2014) Surgical management of trigeminal neuralgia: use andcost-effectiveness from an analysis of the Medicare claims database.Neurosurgery 75:220-226.
- Kang IH, Park BJ, Park CK, Malla HP, Lee SH et al. (2016)A clinical analysis of secondary surgery in trigeminal neuralgia patients whofailed prior treatment. J Korean Neurosurg Soc 59:637-642.
- Noorani I, Lodge A, Vajramani G, Sparrow O (2016)Comparing percutaneous treatments of trigeminal neuralgia: 19 years ofexperience in a single centre. Stereotact Funct Neurosurg 94:75-85.
- Huang CF, Chiou SY, Wu MF, Tu HT, Liu WS (2010) GammaKnife surgery for recurrent or residual trigeminal neuralgia after a failedinitial procedure. J Neurosurg Suppl 113:172-177.
- Berger I, Nayak N, Schuster J, Lee J, Stein S et al.(2017) Microvascular decompression versus stereotactic radiosurgery fortrigeminal neuralgia: a decision analysis. Cureus 9:10.7759.
- Chan MD, Shaw EG, Tatter SB (2013) Radiosurgicalmanagement of trigeminal neuralgia. Neurosurg Clin N Am 24:613-621.
- Kano H, Kondziolka D, Yang HC, Zorro O, Lobato-Polo J etal. (2010) Outcome predictors after gamma knife radiosurgery for recurrenttrigeminal neuralgia. Neurosurgery 67:1637-1644.
- Pollock BE (2006) Radiosurgery for trigeminal neuralgia:is sensory disturbance required for pain relief? J Neurosurg 105:103-106.
- Kondziolka D,Lacomis D, Niranjan A, Mori Y, Maesawa S et al. (2000) Histological effects oftrigeminal nerve radiosurgery in a primate model: implications for trigeminalneuralgia radiosurgery. Neurosurgery 46:971-976.
- Tuleasca C, Carron R, Resseguier N, Donnet A, Roussel P etal. (2012) Patterns of pain-free response in 497 cases of classical trigeminalneuralgia treated with gamma knife surgery and followed up for least 1 year. JNeurosurg 117 Suppl:181-188.
- Niranjan A, Lunsford LD (2016) Radiosurgery for themanagement of refractory trigeminal neuralgia. Neurol India 64:624-629.
- Wang DD, Raygor KP, Cage TA, Ward MM, Westcott S et al.(2018) Prospective comparison of long term pain relief rates after first-timemicrovascular decompression and stereotactic radiosurgery for trigeminalneuralgia. J Neurosurg 128:68-77.
- Regis J, Metellus P, Hayashi M, Roussel P, Donnet A et al. (2006)Prospective controlled trial of gamma knife surgery for essential trigeminalneuralgia. J Neurosurg 104:913-924.
- Zakrzewska JM, Akram H (2011) Neurosurgical interventions for thetreatment of classical trigeminal neuralgia. Cochrane Database of SystematicReviews Article:CD007312..
- Karam SD, Tai A, Wooster M, Rashid A, Chen R et al. (2014)Trigeminal neuralgia treatment outcomes following gamma knife radiosurgery witha minimum 3-year follow-up. J Radiat Oncol 3:125-130.
- Tempel ZJ, Chivukula S, Monaco EA, Bowden G, Kano H et al. (2015)The results of a third gamma knife procedure for recurrent trigeminal neuralgia.J Neurosurg 122:169-179.
- Tuleasca C, Carron R, Resseguier N, Donnet A, Roussel P et al.(2014) Repeat gamma knife surgery for recurrent trigeminal neuralgia: long termoutcomes and systematic review. J Neurosurg 121 Suppl:210-221.
- Helis CA, Lucas JT, Bourland JD, Chan MD, Tatter SB et al. (2015)Repeat radiosurgery for trigeminal neuralgia. Neurosurgery 77:755-761.
- Flickinger JC, Pollock BE, Kondziolka D, Phuong LK, Foote RL et al.(2001) Does increased nerve length within the treatment volume improvetrigeminal neuralgia radiosurgery? A prospective double-blind, randomizedstudy. Int J Radiat Oncol Biol Phys 51:449-454.
- Pollock BE, Phuong LK, Foote RL, Stafford SL, Gorman DA (2001) Highdose trigeminal neuralgia radiosurgery associated with increased risk oftrigeminal nerve dysfunction. Neurosurgery 49:58-64.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences