Percutaneous Neurolysis with Continuous Radiofrequency Energy for the Treatment of Symptomatic Sacroiliac Joints: Study of Clinical Safety and Efficacy
DK Filippiadis, G Velonakis, A Mazioti, C Konstantos, E Brountzos, N Kelekis and A Kelekis
DOI10.21767/2471-9633.100020
Radiology Department, University General Hospital “ATTIKON”, Athens, Greece.
- *Corresponding Author:
- Dimitrios K Filippiadis
Diagnostic and Interventional Radiology
2nd Radiology Department, University General Hospital "ATTIKON"
Medical School, National and Kapodistrian University of Athens
1 Rimini street, 12462 Haidari/ Athens, Greece.
Tel: +30 210 5831812
Fax: +30 2105326418
Email:dfilippiadis@yahoo.gr
Received date: December 08, 2016; Accepted date: December 23, 2016; Published date: December 31, 2016
Abstract
Purpose: To prove safety and efficacy of percutaneous neurolysis with continuous radiofrequency energy for the treatment of symptomatic sacroiliac joints in a series of consecutive patients.
Materials and methods: During the last 2 years, 15 patients suffering from low back pain due to degenerative disorder of the sacroiliac joint underwent percutaneous neurolysis with continuous radiofrequency energy. Under extended local sterility and fluoroscopy 4 cannulas were placed along the sacral foramina and at the L5- S1 level and neurolysis session was performed post motor and sensory evaluation test. NVS pain scores prior and post therapy were compared using Paired Samples t-Test and Wilcoxon Signed Rank Test.
Results: Mean pain score prior to any therapy was 8.05±1.449 NVS units. Mean pain score post therapy was 2.37 ± 2.715, 2.42 ± 2.754, 2.70 ± 2.928 and 3.55 ± 2.837 NVS units at 1, 6, 12, 24 months. The comparison of the patients’ selfreported outcomes concerning pain reduction and mobility improvement prior and post therapy is statistically significant (p<0.001). No complication was noted.
Conclusion: Percutaneous neurolysis with continuous radiofrequency energy seems to be a safe and efficient technique for the treatment of symptomatic, sacro-illiac joints resulting in significant pain reduction and mobility improvement. Proper patient selection is a prerequisite for high success rate.
Keywords
Sacroiliac joint; Pain; Neurolysis; Nadiofrequency; Fluoroscopy.
Introduction
Sacroiliac joint is a diarthrosis between the sacral and the iliac bones which consists of two parts: An articular surface with synovial capsule located anterior and the sacral tuberosity located posterior [1]. Sacroiliac joint ligaments include the interosseous, the short posterior and the long posterior sacroiliac ligaments [2]. Innervation to the sacroiliac joint is provided by sensory fibers from the lateral branch nerves of S1, S2 and S3 posterior rami and the L5 posterior ramus [1, 2].
The sacroiliac joint accounts for approximately one third of chronic low back pain or upper buttock pain cases [1]. Sacroiliac joint pain originates either from the joint itself or from extraarticular structures (e.g. the ligaments). Patients complain of unilateral or bilateral low back or upper buttock pain without radicular component; this pain is exacerbated with manual provocation tests including compression, distraction and torsion of the joint whilst clinical diagnosis is based upon exclusion of low back pain causes, definition of pelvic girdle pain and definition of joint’s stability according the European guidelines for the diagnosis and treatment of pelvic girdle pain [1-3]. Therapeutic armamentarium includes conservative therapy (antiinflammatory and analgesic drugs, physiotherapy), intra-articular injections with a mixture of long acting corticosteroid and local anesthetic, percutaneous neurolysis using cryoablation or RF ablation and minimally invasive or surgical fixation techniques. Percutaneous RF denervation can be applied either at the joint itself or along the sacral foramina where the lateral branch nerves enter [4].
Purpose of this study is to prove safety and efficacy of percutaneous neurolysis with continuous radiofrequency energy at the foraminal level for the treatment of symptomatic, sacroiliac joints in a series of consecutive patients.
Materials and Methods
All patients were informed about the technique itself as well as possible benefits and complications and they signed a written consent form to the procedure. Authors have no conflict of interest to declare. No industry support was received for this study.
Patient selection and evaluation
During the last 2 years, 15 patients (10 female, 5male, mean age 58.33 ± 4.806) suffering from unilateral or bilateral low back or upper buttock pain without radicular component underwent percutaneous neurolysis with continuous radiofrequency energy for the treatment of symptomatic, sacroiliac joints. All patients had undergone different conservative therapies without success. In our study, pre-enrolment conservative therapy was not prespecified in the protocol but potentially included the following: use of non-steroidal anti-inflammatory drugs and opioid analgesics and chiropractic care. All patients underwent a positive diagnostic block 1 week prior to the neurolysis session.
Each patient underwent coagulation laboratory tests and physical examination including manual provocation tests prior to the percutaneous neurolysis session. Evaluation of all imaging studies in correlation with the patients’ medical record was performed before each procedure. Pre operational imaging included X-Rays, CT or multiplane MRI. Exclusion criteria for the procedure included untreatable coagulopathy, active, systemic or local infections and patient unwilling to consent to the procedure.
Percutaneous neurolysis session
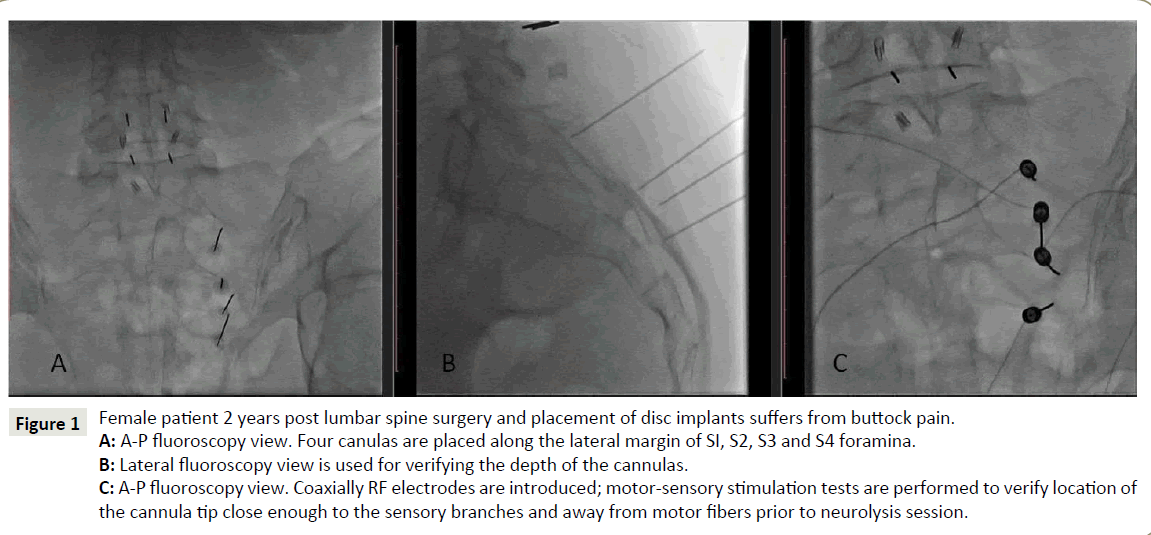
Under extensive local sterility, local anesthesia and fluoroscopic guidance, 4 canullas were percutaneously placed along the lateral margin of S1, S2, S3 and S4 sacral foramina and a fifth one at the level of lumbar L5 posterior ramus (Figures 1 and 2). Correct cannula location was verified in A-P and lateral views. Coaxially a RF electrode was introduced and motor-sensory stimulation tests were performed to verify location of the cannula tip close enough to the sensory branches and away from motor fibers. Following successful stimulation tests electrode was withdrawn and a small amount of local anesthetic was injected. Coaxially the electrodes were re-inserted and 2 ablation session of 90 s at 85-90°C were performed at each level. Patient remained in the hospital for one hour and then discharged.
Outcome measures
Pain and mobility were recorded prior and at 1, 6, 12, 24 months post neurolysis session with clinical evaluation and the Brief Pain Inventory adapted for Greek population [5]. This inventory includes questions concerning the pain itself and its influence upon patient's activity (sleep, occupation and housework, walking) and mobility impairment.
Follow-up consisted of clinical visits (general, clinical and neurological condition, pain reduction and mobility improvement according to NVS scale) at 1, 6, 12, 24 months post the treatment session. Questions asked during the follow-up period concerned the pain reduction and mobility improvement and whether the procedure had decrease or totally relieve the symptoms they were treated for.
Figure 1: Female patient 2 years post lumbar spine surgery and placement of disc implants suffers from buttock pain.
A: A-P fluoroscopy view. Four canulas are placed along the lateral margin of SI, S2, S3 and S4 foramina.
B: Lateral fluoroscopy view is used for verifying the depth of the cannulas.
C: A-P fluoroscopy view. Coaxially RF electrodes are introduced; motor-sensory stimulation tests are performed to verify location of
the cannula tip close enough to the sensory branches and away from motor fibers prior to neurolysis session.
Figure 2: Female patient 2 years post lumbar spine surgery and placement of disc implants suffers from buttock pain (same patient with
Figure 1).
A: Lateral oblique fluoroscopy view (ÃÆâÃâââ¬ÃâÃ
âScottie dogÃÆâÃâââ¬Ãâàprojection): Canula is placed at the sacral ala where the lumbar L5 posterior
ramus lies.
B: Lateral fluoroscopy view is used for verifying the depth of the canula.
Multivariate analysis was performed in order to evaluate the role of confounding factors on final results. For the performance of a power calculation, we considered clinically significant any pain reduction of more than 4 NVS Units. Given a α of 0.05, using an estimated mean pain score of 8 NVS Units prior to the intervention, and a potential sample of 15 patients, the power of our study was calculated 99,9%.
Statistical analysis
Data were summarized using mean value, median value and Standard Deviation. NVS pain scores prior and post therapy were compared using Paired Samples t-Test and Wilcoxon Signed Rank Test. P values <0.05 were considered to indicate a statistically significant difference. Statistical analyses were performed with IBM SPSS Statistics 21.
Results
Percutaneous placement of canulas at the correct locations was feasible in all patients. All patients completed the 24 months follow-up period reporting a clinical satisfactory pain reduction effect.
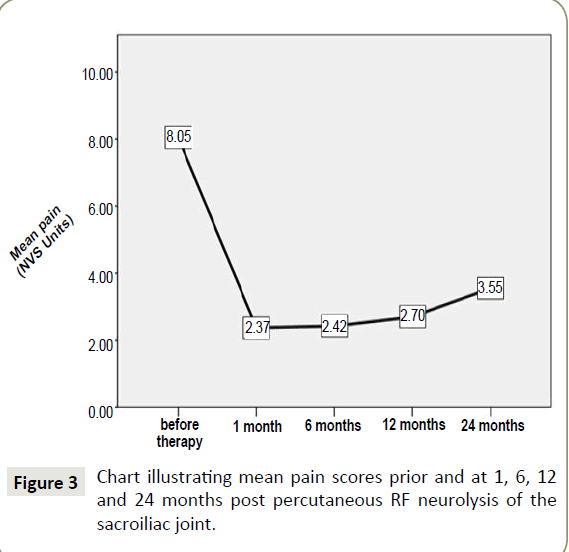
Mean pain score prior to any therapy was 8.05 ± 1.449 NVS units. Mean pain score post therapy was 2.37 ± 2.715 NVS units at 1 month, 2.42 ± 2.754 NVS units at 6 months, 2.70 ± 2.928 NVS units at 12 months and 3.55 ± 2.837 NVS units at 24 months POST therapeutic session (Figure 3). The comparison of the patients’ self-reported outcomes concerning pain reduction and mobility improvement prior and post therapy is statistically significant (p<0.001).
Overall mobility improved in all patients. No clinically significant complications (minor or major) were noted in our study population.
Pain reduction remained statistically significant during the whole follow up period (p<0.001) compared to baseline, with a minimum of 4.5 NVS Units mean pain decrease after 24 months. However, from month 1 to month 24, there was a mean pain increase of 1.17 NVS Units, which was not considered clinically important. Nonetheless, we performed a post-hoc sample size calculation for pain differences during the follow up period, using a power of 80%, which indicated a sample of 91 patients.
Multivariate regression analysis revealed no significant association between pain decrease and age (p=0.718), weight (p=0.892) and height (p=0.2). No statistically significant difference on pain reduction was noticed between men and women (p=0.545).
Discussion
Pain originating from sacroiliac joint can be due to either irritation of the joint’s synovium or irritation of the innervating nerves by means of chemical mediators. Although imaging guided steroid infiltrations report an immediate pain relief in 50-90% of patients for 10 ± 5 months, in case of short lived improvement, one should opt for percutaneous neurolysis [2]. Unfortunately due to widespread methodological flaws and a literature paucity concerning the evaluation role of both diagnostic and therapeutic interventions the evidence for radiofrequency neurotomy (else called denervation) is limited [6, 7].
Percutaneous denervation can be applied either at the joint itself or by creating a semi-circular ablation zone laterally to the posterior sacral foramina at the entrance level of the lateral branch nerves. Alternatively a strip-like linear ablation zone can be formed lateral to the foramina. Prior to any neurolysis session and at least 48 h before a diagnostic anesthetic block should be performed to verify sacroiliac joint as the pain source. Imaging guidance is a prerequisite for correct canula placement; fluoroscopy and ultrasound are the most commonly used modalities [8-10]. Cone beam fluoroscopy can provide CT like 3D reconstructions acting as a problem solver in obese patients or other difficult situations; alternatively navigation and reconstruction systems may also be used to facilitate multiplanar imaging of ultrasound-guided injections [11, 12].
Compared to other studies in the literature using continuous radiofrequency energy, a significant pain reduction and mobility improvement effect are reported in our results as well [13-16]. Apart from continuous, pulsed radiofrequency mode has been used in sacroiliac joint as well [17]. This is an alternative for pain management offering control without significant damage to nervous tissue and without the risk of motor deficit. The technique uses pulses of RF energy aiming at localized voltage fluctuations without excessive heating (temperature remains below 41°C. Using pulsed radiofrequency, neuromodulation rather than neurodestruction inhibits the evoked synaptic activity.
Pelvic girdle pain due to sacroiliac joint pathology (and/or degeneration) can be a chronic condition affecting not only mobility but life quality as well. The management of such chronic diseases requires a more active patient role in the management decisions along with a patient-care provider collaboration which will involve effective treatment, self-management education and follow-up [18]. In such circumstances, the incorporation of care managers (specifically trained nurses) who will directly work with the patients assisting them in lifestyle changes performance and improvement of compliance with care recommendations will result in better disease control [18].
Limitations of our study include the small patient sample and the lack of a control group which will consist of patients undergoing conservative therapy or intra-articular injections and will be randomized and prospectively compared. Additionally there was no comparison between continuous and pulse RF application in the sacroiliac joint.
Conclusion
Percutaneous neurolysis with continuous radiofrequency energy seems to be a safe and efficient technique for the treatment of symptomatic, sacro-illiac joints resulting in significant pain reduction and mobility improvement. Proper patient selection is a prerequisite for high success rate.
References
- Forst SL, Wheeler MT, Fortin JD, Vilensky JA (2006) The sacroiliac joint: Anatomy, physiology and clinical significance. Pain Physician 9: 61-67
- Organ LW, Burnham RS, Avila AJ, Agur AM. Radiofrequency denervation of the sacroiliac joint. DIROS/OWL RF Monograph SIJ ver 6.0, pp: 2-7.
- Vleeming A, Albert HB, Ostgaard HC, Sturesson B, Stuge B (2008) European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur Spine J 17: 794-819.
- Kelekis A, Filippiadis D (2014) Sacroiliac joint injections. In: Mauro et al., Image guided interventions 2nd Edition. Elsevier Saunders Philadelphia, pp: 1241-1243.
- Mystakidou K, Mendoza T, Tsilika E, Befon S, Parpa E (2001) Greek brief pain inventory: Validation and utility in cancer pain. Oncology 60: 35-42.
- Hansen HC, McKenzie-Brown AM, Cohen SP, Swicegood JR, Colson JD, et al. (2007) Sacroiliac joint interventions: A systematic review. Pain Physician 10: 165-184.
- Rupert MP, Lee M, Manchikanti L, Datta S, Cohen SP (2009) Evaluation of sacroiliac joint interventions: A systematic appraisal of the literature. Pain Physician 12: 399-418.
- Andreula C, Muto M, Leonardi M (2004) Interventional spine procedures. Eur J Radiol 50: 112-9.
- Yin W, Willard F, Carreiro J, Dreyfuss (2003) Sensory stimulation guided SIJ RF neurotomy: Technique based on neuroanatomy of the dorsal sacral plexus. Spine 28: 2419-2425.
- Narouze SN (2011) Atlas of ultrasound guided procedures in interventional pain management. Sonoanatomy of the sacrum ans sacroiliac joint. Moriggl B Ch 5: 103-105
- Kelekis A, Filippiadis D (2013) Percutaneous therapy versus surgery in chronic back pain: How important is imaging in decision-making? Imaging in Medicine 5; 187-196
- Filippiadis DK, Kelekis A (2016) A review of percutaneous techniques for low back pain and neuralgia: Current trends in epidural infiltrations, intervertebral disk and facet joint therapies. Br J Radiol 89: 20150357.
- Ferrante FM, King LF, Roche EA, Kim PS, Aranda M, et al. (2001) Radiofrequency sacroiliac joint denervation for sacroiliac syndrome. Reg Anesth Pain Med 26: 137-142.
- Gevargez A, Groenemeyer D, Schirp S, Braun M (2002) CT-guided percutaneous radiofrequency denervation of the sacroiliac joint. Eur Radiol 12: 1360-1365.
- Buijs EJ, Kamphuis ET, Groen GJ (2004) Radiofrequency treatment of sacroiliac jointrelated pain aimed at the first three sacral dorsal rami: A minimal approach. Pain Clinic 16: 139-146.
- Burnham RS, Yasui Y (2007) An alternate method of radiofrequency neurotomy of the sacroiliac joint: A pilot study of the effect of pain, function and satisfaction. Reg Anesth Pain Med 32: 12-19.
- Vallejo R, Benyamin RM, Kramer J, Stanton G, Joseph NJ (2006) Pulsed radiofrequency denervation for the treatment of sacroiliac joint syndrome. Pain Med 7: 429-434.
- Ciccone MM, Aquilino A, Cortese F, Scicchitano P, Sassara M, et al. (2010) Feasibility and effectiveness of a disease and care management model in the primary health care system for patients with heart failure and diabetes (Project Leonardo). Vasc Health Risk Manag 6: 297-305.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences