Transpedicular Surgical Decompression of Dorsal Spinal Tuberculosis (Pottas Disease) with Vertebral Collapse without Fixation
Deepak K Jha, Rahul Singh, Ishita Pant, Mukul Jain, Suman Kushwaha and Rima Kumari
DOI10.21767/2471-9633.100011
Institute of Human Behavior and Allied Sciences, Delhi, India
- Corresponding Author:
- Dr. Deepak Kumar Jha
Department of Neurosurgery
IHBAS, Delhi- 110095, India
Tel: +919868527900
E-mail: jhadeepak2@rediffmail.com
Received date: March 21, 2016; Accepted date: April 15, 2016; Published date: April 22, 2016
Citation: Jha DK, Singh R, Pant I. Transpedicular Surgical Decompression of Dorsal Spinal Tuberculosis (Pott’s Disease) with Vertebral Collapse without Fixation. Neurosurg.2016, 1:2. doi:10.21767/2471-9633.100011
Abstract
Introduction: Spinal tuberculosis is prevalent in developing countries. Advancements in technique and technology has improved the outcome, but cost of the newer prosthetic implants and insufficient public healthcare infrastructure in third world countries pose difficulty in surgical treatment of many of these patients.
Methods: Twenty two patients of dorsal Pott’s disease having anterior or anterolateral compressionswith significantneurologicaldeficitswereprospectively studied in five years period (2010 to 2015) and were subjected to unilateral transpedicular decompression of the dorsal cord with maximal preservation of bony elements including ribs without fixation by prosthetic implants. Patients were advised absolute bed rest for 3 months after surgery.
Results: Study group included 12 males and 10 females of with average age 37.5 years (range 14 to 68 years). Clinical improvement was observed in all but one patient, who showed recovery in the follow up. Three patients had recurrence with neurological deterioration due to discontinued antitubercular chemotherapy and required second surgery leading to clinical recovery. There was no increase in kyphosis in follow up in any patient.
Conclusion: Unilateral transpedicular decompression with bed rest for three months appear an option in selected patients of dorsal Pott’s disease with anterior/ anterio-lateral compression with significant neurological deficit.
Keywords
Dorsal spine; Spinal tuberculosis; Pott’s disease; Spinal fixation; Kyphosis
Introduction
Tuberculosisof spine is prevalent in developing countries and is considered a disease affecting people from low socioeconomic groups [1-9]. Over the period of last three to four decades, chemotherapy for tuberculosis and various advanced surgical options which include fixation of the spinal segments with newer prosthetic implants have changed the outlook [1,10]. Another new development in the field of prosthetic implants for spinal surgeries has occurred: increasing use of Magnetic Resonance (MR) imaging compatible and internationally acceptable implants (made of titanium or bio-degradable materials), which are very costly and simultaneous phasing out of older and cheaper implants (made of stainless steel) [1,11-13]. This has led to a strange situation for the patients of spinal tuberculosis because they cannot afford the cost of the implants even if they get a chance of admission in poorly financed public sector hospitals which do not provide free prosthetic spinal or for that matter any costly prosthetic implants [14-17]. Unlike other levels, sternum and rib cage provide additional stability to the thoracic spine, and this additional support to the thoracic spine may help in selecting surgical approach for treatment of spinal tuberculosis of dorsal spine [18]. Role of decompressive surgery along with various methods of fixation in a patient of dorsal Pott’s disease with vertebral collapse and cord compression with significant neurological deficit is explicitly accepted in the literature; however, reports of decompressive surgery alone in dorsal Pott’s disease with vertebral collapse are rare [19-21]. We report prospective study of a series of 22 patients of dorsal Pott’s disease with vertebral collapse, in which decompressive surgery without fixation, with preservation of ribs and most of the posterior elements, was used as a method of treatment and discuss our findings.
Material and Methods
Study was carried out at a centre, where advanced facilities like image intensifier required for pedicle screw placements are not available. Intra-operative Mobile X ray (Allenger, 150 mA) or preoperative ‘marker X-ray’ was used for spinal level localization.
Selection criteria
1. Patients with radiological (MR/CT imaging) signs of destructive lesions of thoracic vertebral body/ies with anterior or antero-lateral cord compression due to bony wedge, liquid and soft tissue along with clinical features suggestive of, or already diagnosed cases by pus examination of tubercular infection of thoracic vertebra/e.
2. Progressive neurological deficit with Frankel Scales [22] A, B or C.
3. Patients who agreed to give consent to undergo their surgeries with the available facilities. They were explained about the other options of surgical treatments which includes fixation by prosthetic implants in addition to decompression and fusion.
4. Patients who agreed for absolute bed rest for 3 months or more after surgery. ‘Absolute bed rest’ was defined as all daily activities including toilet functions to be performed on bed and sitting or standing was not allowed.
Exclusion criteria
1. Patients with Frankel scales D and E who showed progressive clinical improvement on conservative treatment (ATT and absolute bed rest).
2. Cobb’s angle more than 40 degrees.
3. HIV positive patients and patients with active and symptomatic other system involvement in addition to brain and spine. These patients need multidisciplinary treatment and only facilities pertaining to neurosciences are available at our institute.
4. Patients who opted for decompressive surgery with fusion and fixation by prosthetic implants and were referred to other centre with required facilities.
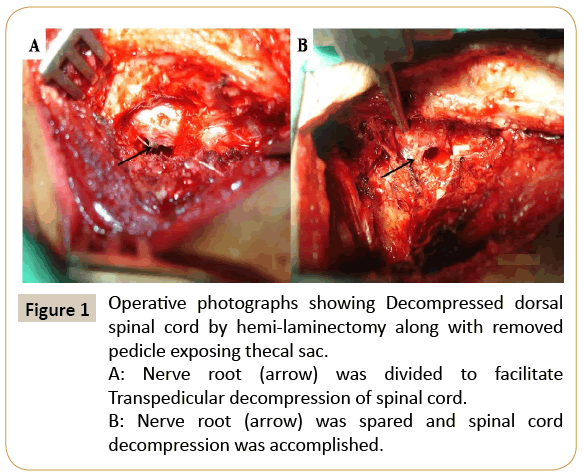
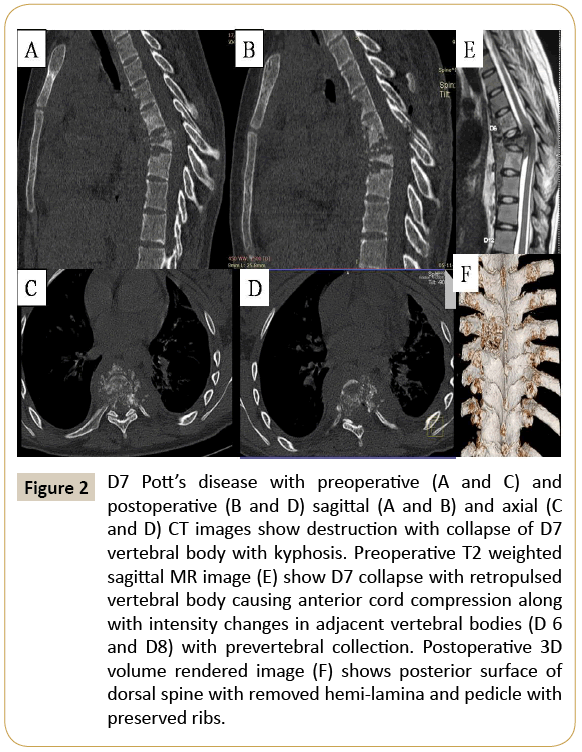
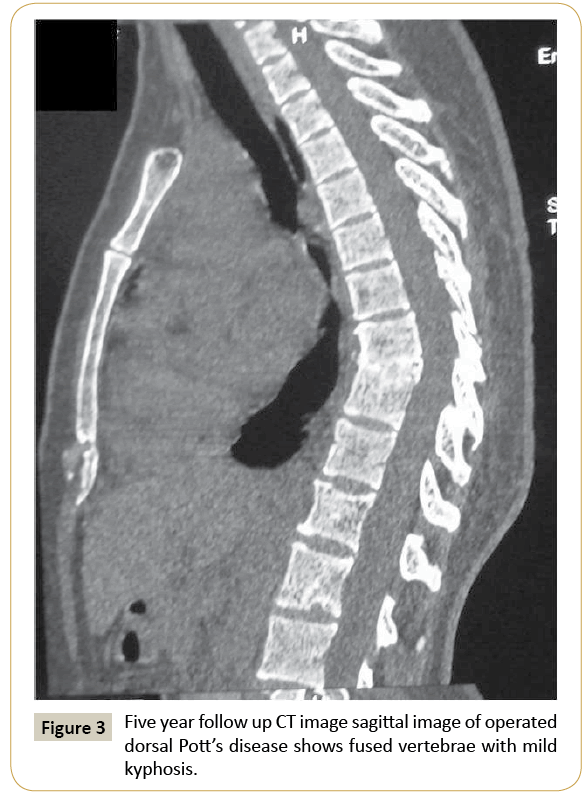
All the patients were evaluated by detailed clinical examination, chest radiographs and three consecutive morning’s sputum examinations for acid fast bacilli, wherever needed. Four-drug Anti Tubercular Chemotherapy (ATT) was started if patient was not taking it already. Spinal imaging was done by plain radiograph, CT and MR imaging of the spinal region of interest. Preoperative Cobb’s angle for assessment of kyphosis was recorded. Side (Right or left) of the surgical approach through more affected side was decided based on clinical and radiological evidence of compressing lesion such as granulation tissue/pus and wedge of vertebral body. Left side was selected, where clinical and radiological signs were symmetrical. Transpedicular decompression of the spinal canal was done for anterior and antero-lateral compressions with or without hemi-laminectomy. Patients were operated in prone positions under general anesthesia with bolsters under chest and hip. More affected side based on clinical and radiological findings were chosen for transpedicular surgeries. Midline vertical incisions were given based on either pre-operative marker X ray or intra-operative mobile X ray. Ipsi-lateral hemi-laminae, pedicles, transverse processes were exposed, which occasionally needed limited horizontal division of paraspinal muscles near midline. Ipsi-lateral hemi-laminectomy (for decompression of lateral granulation tissue) and removal of affected pedicle/s (for anterior and anterolateral decompression of granulation tissue) were performed by electric drill, chisel and hammer, bone nibblers, kerrison punches and curettes. Posterior surfaces of medial part of ribs were exposed but were not removed. Root exiting from spinal canal was rarely sacrificed only if it obstructed decompression of anteriorly situated compressing bony elements (Figure 1A). Granulation tissue anterior and around the exiting nerve root were gradually removed in piecemeal to avoid division of the nerve root (Figure 1B). Adequate portions of transverse process, pedicle and ipsilateral lamina were removed just sufficient to gain access to bony or soft tissue compressing the spinal cord without manipulating the cord itself. Cavity by scooping or drilling was made under the compressing bony element which allowed the space for pushing down the thinned out bony part or granulation. Surgical goal was only decompression of cord and all bony elements were preserved as much as possible. (Figures 1 and 2) Reduction of kyphosis was not actively done; however, prone position with bolsters under chest and hip apparently led to minor degrees of reduction, which was maintained postoperatively by ‘absolute bed rest’ on flat and hard foam-bed in postoperative period. Patients were not allowed to sit or stand for 3 months after surgery, but active limb and chest physiotherapy were continued. Pain was recorded as per Visual Analog Scale (VAS) of 100 and was assessed for rest pain, pain on turning on bed and pain on mild thumping over the operative site three weeks after surgery only when there was no pain on turning on bed [23]. During hospital stay, relatives of patients were trained for physiotherapy maneuvers possible at home and assessment and recording of pain once daily as per VAS. Patients were discharged two weeks after surgery and were advised to record pain once daily (with the help of relative) after discharge and attend out-patient department 3 months after surgery. Patients were evaluated after three months by plain radiograph and CT scan for assessment of bony fusion and duration and severity of pain persisted after surgery. If there was no pain on sitting, mobility was allowed. In patients, who had back pain on sitting after three months, were advised absolute bed rest for 1 more month. Patients were followed up at 3 and 6 months after surgery then at yearly intervals. CT scans of the dorsal spine were done after 24 hours of surgery and after 3 months, and then at yearly intervals for assessment of bony fusion and kyphosis (Figures 2 and 3).
Figure 1: Operative photographs showing Decompressed dorsal spinal cord by hemi-laminectomy along with removed pedicle exposing thecal sac.
A: Nerve root (arrow) was divided to facilitate Transpedicular decompression of spinal cord. B: Nerve root (arrow) was spared and spinal cord decompression was accomplished.
Figure 2: D7 Pott’s disease with preoperative (A and C) and postoperative (B and D) sagittal (A and B) and axial (C and D) CT images show destruction with collapse of D7 vertebral body with kyphosis. Preoperative T2 weighted sagittal MR image (E) show D7 collapse with retropulsed vertebral body causing anterior cord compression along with intensity changes in adjacent vertebral bodies (D 6 and D8) with prevertebral collection. Postoperative 3D volume rendered image (F) shows posterior surface of dorsal spine with removed hemi-lamina and pedicle with preserved ribs.
Results
Patient characteristics
Forty six symptomatic patients of spinal tuberculosis were treated by us in last 5 years (January 2010 to February 2015), out of which 39 needed surgical interventions. There were 26 patients who had dorsal spinal tuberculosis who needed surgical treatment. Out of these 26 patients, 4 had posterior compressions due to extradural granulation tissue, pus and destructed spine/laminae without spinal instability and were treated by laminectomies. Remaining 22 patients, who had anterior/antero-lateral compressions due to pus, granulation tissue and wedging of vertebral bodies due to collapse, formed the study group. There were 12 females and 10 males with ages ranging from 14 to 68 years with average age 37.5 years. All these patients belonged to low socioeconomic group and failed to get admissions at other public sector hospitals/institutes with advanced facilities. Clinical characteristics along with their preoperative Frankel Scales are summarized in the Table 1.
Clinical features
Symptom duration was 15 days to 2 years (average 5.29 months). Commonest symptom was back pain followed by motor deficit (n=22), sensory deficit (n=21), bladder bowel involvement (n=17). Respiratory difficulty (n=2) and pressure sores (n=1) over sacrum, iliac crest and heel were observed in a total of 2 patients. Preoperatively patients were in Frankel scale grades A (n=5), B (n=13) and C (n=4). Other system involvements by tuberculosis were observed in six patients. It included cervical lymph node involvement (n=1), pulmonary involvement (n=4) and simultaneous involvement of abdomen, second lumbar vertebra and brain in the form of meningitis (n=1) 8 months prior to admission. Two patients (case 15 and 22) were diagnosed cases of atypical mycobacterial infection and were on second line ATT drugs for last 10 days to 2 months for tubercular infection of lung (n=1) and brain (tubercular meningitis) (n=1) respectively. Three patients (case number 5, 6 and 11) discontinued ATT without medical advice 2 months after surgeryonce they significant improved neurologically. All these three patients started walking after 2 months and came back after 8 and 12 months with reappearance of symptoms to preoperative levels. They were subjected to surgical decompression again at the same levels due to re-accumulation of pus, granulation tissue and increase in kyphosis. One patient (case 10) had ATT induced acute and severe hepatitis and had shown deterioration after surgery (Frankel scale C to A). ATT was discontinued for 3 weeks, after which, his liver function parameters became normal. Gradual introduction of ATT drugs one by one at the interval of 5-7 days was done. Improvement in neurological symptoms was observed only after 12 weeks. Another patient (case 17), with preoperative Frankel scale A, did not show any neurological improvement till 8 weeks after surgery. Patient could improve up to Frankel scale C at the end of 6 months and is able to walk with mild spasticity with continent bladder/bowel functions at the end of 2 years.
Radiological findings
CT and MRI evaluation of spine revealed involvement of one level in 2, two contiguous levels in 14 and three contiguous levels in remaining 6 patients. Lateral columns (pedicles and facet joints) were involved in all the cases with unilateral involvement in 17 and bilateral involvement in remaining 5 patients. Preoperative Cobb’s angle ranged from 11° to 36° (average 25°). There was minimal change in the Cobb’s angle in early (24-48 hours after surgery) or after 3-6 months CT images of spine, except in three cases that needed re-surgery and the change was less than 5°. At second pre-operative assessment, three patients who had discontinued their ATT, Cobb’s angle had increased 14° (case 5), 8° (case 11) and 11° (case 6) in comparison to immediate first post-operative assessments done 24 hours after surgery. Barring three patients mentioned above, postoperatively, none of the patients had radiological features suggestive of progression in their kyphosis during their follow up CT scan imaging.
ATT Chemotherapy
Nineteen patients were being treated preoperatively by ATT for 1 week to 1 year duration. In remaining 3 patients ATT was started after admission. Two patients had their sputum positive for Mycobacterium. Three patients were already diagnosed having atypical Mycobacterial infection by examination of pus by needle aspiration at other center and were being treated by second line ATT, which was continued postoperatively for a total period of 2 years. Remaining patients (n=19) were treated by 4-first line ATT for 3 months followed by 3-drug first line ATT for remaining 15 months.
Surgical results
A total of 25 surgical procedures in 22 patients were carried out which included three patients who were re-operated for recurrences of their lesions due to discontinuation of ATT.
First clinical improvement after surgery was observed as reduction in spasticity of lower limbs. Barring one, all patients showed progressive improvements in back pain, motor and sensory deficits of lower limbs and bladder/bowel functions postoperatively. Remaining one patient with Frankel grade C deteriorated clinically postoperatively and developed flaccid paraplegia with simultaneous acute ATT induced hepatitis. Conservative treatment with discontinuation of Rifampicin and Pyrizinamide for a period of 12 weeks led to recovery of hepatitis followed by progressive recovery in neurological functions. Postoperative pain in patients without root division (n=15) was moderate (VAS 45–74 mm) for first 48 hours, which required parenteral analgesics (50 mg of intramuscular Diclofenac sodium) followed by oral analgesics for further 48-72 hours. Seven patients, whose single roots were divided to aid decompression in earlier part of the study, had severe post-operative pain on the side of the surgery (VAS 75–100 mm) for first 72-96 hours akin to neuropathic pain which only partially responded to parenteral analgesics along with oral Baclofen or Amytriptiline followed by moderate to severe pain (VAS 45-74 mm) for 1-2 weeks. Oral medications for neuropathic pain had to be continued for 3-6 weeks after surgery. After experience of initial few cases, we avoided dividing root for aiding decompression and it was possible at the cost of some extra operative time in the range of 15 to 30 minutes (Figure 1B). Patients were sent home two weeks after surgery. Pain while turning on bed was assumed as an indirect indication of instability and it was relieved in most of the patients over a period of 6-8 weeks. Pain on mild thumping over operative site was absent in all the cases by the end of 10 weeks. Three patients were advised 1 month more bed rest as they complained of back pain on sitting after 3 months’ bed rest. Barring three, all patients (n=19) reported to out-patient clinic for follow up visits at 3 months, revealed clinical improvements. Three patients, who did not turn up at 3-month follow up, had discontinued ATT 6-8 weeks after surgery once they started walking but deteriorated again and came back after 8-12 months with Frankel grade A.
Histo-pathological examinations of granulation tissue was conclusive in all the patients (n=22). Excluding three patients diagnosed of atypical mycobacterial infection at other center, AFB staining and culture and sensitivity of mycobacteria in pus from the lesions were positive in three patients.
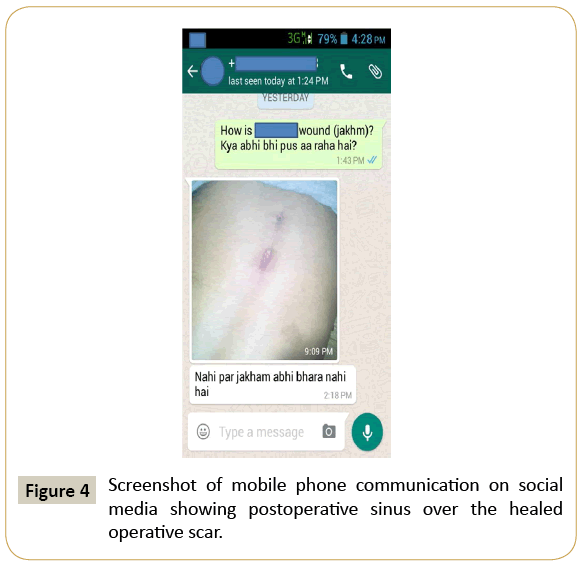
Complication
Postoperative cold abscess formation at the operative site 4 weeks after surgery was seen in one patient. It led to chronic pus discharging sinus which gradually healed over a period of 8 weeks (Figure 4). Three patients discontinued ATT after 2 months and lost to follow up till they deteriorated again, which may be due to insufficient information provided from our end, lack of awareness, illiteracy and poverty due to which they had to pursue their jobs for their livelihoods.
Follow up
Patients were followed up at 3, 6 and 12 months after surgery and then at yearly intervals. No patient was advised to attend outpatient clinic before 3 months and relatives were instructed to communicate any difficulty/problem/query personally, telephonically or through social media applications of mobile phones (Figure 4) mainly due to difficulty in transportation of patients on absolute bed rest. Follow up periods ranged from 13 months to 5 years (average 22 months) (Figure 3). Overall 18 patients improved to Frankel grade E. Remaining 4 patients are in Frankel grade C (n=1) and D (n=3). Two out of 3 patients in Frankel grade D are still improving in their follow up periods. No patient had shown increment in their kyphosis.
Discussion
Recent advancements of technologies in neurosurgical equipments and techniques have changed the outcome of some of previously surgically untreatable spinal conditions [24-32]. Video-assisted thoracoscopic surgeries, anterior and anterolateral transthorasic, retroperiotoneal and posterior approaches along with newer prosthetic implants have left no dorsal spinal condition untreatable surgically [16,17,19,28,32,33]. However there is another extreme of the spectrum in developing countries where many poor patients are left untreated due to lack of adequate infrastructure (number of beds/hospitals), human resource (medical and paramedical staff), literacy/awareness and capacity to afford cost of implants at public healthcare facility or cost of treatment at private healthcare facility [2,3,14,34-42]. Medical practice in this era is expected to be ethical; evidence based and should adhere to various protocols established over the years for quality and safety. Therefore, if a paraplegic patient with tuberculosis of dorsal spine with kyphosis is to be treated, he has to be operated at a center where at least radiographic localization equipment, high speed drill, and surgeons are available. Tuberculosis is prevalent in developing countries and burden of spinal tuberculosis patients, who are extremely poor, is much more than what public sector hospitals in developing countries can handle/treat. (1-9) Even if a poor patient is admitted to a public sector hospital, cost of prosthetic implants is beyond his reach. Average cost of available implants required for a patient of dorsal spinal tuberculosis of 1-2 levels is approximately USD 1000, which is more than or equal to annual income of most of these patients [1,11-13,16]. There are regulations/means/ facilities provided by various governmental schemes of which seldom reach to these needy patients due to array of system/ administration related problems [41-44]. Unfortunately, the end result is to choose ATT alone (without surgery) or effective decompressive surgeries without fixation through minimum surgical trauma and prolonged bed rest for bony fusion to occur. Wound healing is always a problem in these patients as most of them are in poor nutritional state [9,16].
There is no consensus or established guideline for surgical treatment of dorsal spinal tuberculosis, but there are sufficient reports available to suggest that progressive and significant neurological deficit with radiological evidence of cord compression should be treated by surgery [11,45-54] There are rare reports of decompressive surgery alone without fixation but there is no mention of additional stability provided to dorsal spine by rib cage as a supporting reason for this approach [18,19,49]. Progressive kypho-scoliosis and neurological deterioration are likely complications, if unstable spine is not fixed [11,44,55-59]. Absolute bed rest appears to eliminate load on the diseased spine/vertebrae which led to no increase in the kyphosis in our study group in the post-operative period and follow up. External brace as a method of reducing mobility and preventing kyphosis have been used earlier. They seem to reduce mobility in addition to rib-cage and sternum but its role in reducing load over the vertebral body imparted by erect posture while sitting or standing is doubtful [19,49]. Maximum Cobb’s angle in our study was 36° and we feel that Cobb’s angle of more than 40° should not be operated without fixation.
Postero-lateral approaches to the dorsal spine mention division of exiting nerve root at one or more than one level, resection of medial part of ribs along with transverse process and pedicle to aid decompression, which was experienced by us also [19,40]. However, severity of post-operative pain despite changing our approach to divide the nerve root (division between two ties or cauterize and divide) led us to attempt nerve root sparing technique. After early difficulty in decompressing spinal cord around the nerve root, it was possible to preserve it in all the cases and decompression was possible by merely retracting nerve root without handling cord at the cost of some extra time in decompression of spinal canal. Leaving maximum bony elements after neural decompression help in ultimate bony fusion once infection is treated by ATT.
Most of the patients of Pott’s spine in developing countries belong to low socio-economic class and have poor nutritional status as in our study too [49,34,60-63] Despite reports of extended costotransversectomy along with fusion for unstable dorsal spine tuberculosis, [19,40,63] we feel that, keeping surgical invasion to minimum will be helpful in avoidance in wound and implant related complication in these poor patients as their preoperative nutritional status affect wound healing [49,62,63]. One of our patients had developed postoperative pus discharging sinus which gradually healed over a period of 8 weeks.
Major issue with our study was compliance for the drugs and absolute bed-rest for three months which is similar to some other reports [41,61]. Two patients of our series, who discontinued ATT after 2 months and started walking, was mainly due to unawareness about the significance, risks and consequence of bed-rest and ATT. Proper patient education by treating medical personnel can’t be overstressed to avoid such problems. Two weeks hospital stay after surgery allows the patient to learn general care, toilet activities on bed and limb and chest physiotherapy by experts. Over the two weeks period, most of the patients experience significant improvements in their neurological functions and that motivates them for further bed-rest. Decompression of spinal cord along with immobilization by prosthetic implants allows better immobilization and early ambulation of these patients and should always be done whenever feasible [9,24,40]. Decompression alone without fixation for dorsal Pott’s disease patients, though not ideal, but is the only method available for a large number of poor patients, especially in developing countries, where Pott’s disease is endemic and free healthcare facilities for all is still a distant goal [14,35-39,41,42].
We conclude that neural decompression with minimal bony removal without spinal fixation is a valid option in selected cases of dorsal Pott’s disease patients who need surgery, till goal of ‘free healthcare for all’ is achieved in developing countries.
Acknowledgement
Authors acknowledge radiological data acquisition by Mr. Narendra K Sharma, Technician, Department of Neuroradiology, Institute of Human Behavior and Allied Sciences, Delhi, India.
References
- Garg RK, Somvanshi DS (2011) Spinal tuberculosis: a review.J Spinal Cord Med 34: 440-454.
- World Health Organization (2011) HIV/TB Facts.
- World Health Organization (2010) 2010/2011 tuberculosis global facts.
- Pawar UM, Kundnani V, Agashe V, Nene A, Nene A (2009) Multidrug resistant tuberculosis of the spine – is it the beginning of the end? A study of twenty-five culture proven multidrug-resistant tuberculosis spine patients. Spine (Phila Pa 1976) 34:E806–E810.
- Talbot JC, Bismil Q, Saralaya D, Newton DA, Frizzel RM, et al. (2007) Musculoskeletal tuberculosis in Bradford - a 6-year review.Ann R CollSurgEngl 89: 405-409.
- N A, Ahmad F, Huda N (2013) Osteoarticular tuberculosis-a three years' retrospective study.J ClinDiagn Res 7: 2189-2192.
- Torres C, Riascos R, Figueroa R, Gupta RK (2014) Central nervous system tuberculosis.Top MagnReson Imaging 23: 173-189.
- Garcia-Monco JC (2014) Tuberculosis.HandbClinNeurol 121: 1485-1499.
- Moon MS (2014) Tuberculosis of spine: current views in diagnosis and management.Asian Spine J 8: 97-111.
- JuttePC , van Loenhout-Rooyackers JH (2006) Routine surgery in addition to chemotherapy for treating spinal tuberculosis. Cochrane Database Syst Rev. 5:CD004532.
- Oguz E, Sehirlioglu A, Altinmakas M, Ozturk C, Komurcu M, et al. (2008) A new classification and guide for surgical treatment of spinal tuberculosis.IntOrthop 32: 127-133.
- Yang L, Liu Z (2013) Analysis and therapeutic schedule of the postoperative recurrence of bone tuberculosis.J OrthopSurg Res 8: 47.
- Agrawal A, Chandra H, Agrawal A, Singhal N, Kumar S (2015) Anterior Versus Posterior Fixation in Thoracic Tubercular Spine. J US-China Med Sci 12:35-39.
- Rao GM, Choudhary M (2012) Health Care Financing Reforms in India.
- N A, Ahmad F, Huda N (2013) Osteoarticular tuberculosis-a three years' retrospective study.J ClinDiagn Res 7: 2189-2192.
- Adeolu AA, Komolafe EO (2014) Outcome of a posterior spinal fusion technique using spinous process wire and vertical strut.Ann Afr Med 13: 30-34.
- Adeolu AA, Komolafe EO, Kolawole OA (2011) The technique of using rigid vertical strut and spinal process wire for posterior spinal stabilization.J Spinal Disord Tech 24: 406-408.
- Watkins R 4th, Watkins R 3rd, Williams L, Ahlbrand S, Garcia R, et al. (2005) Stability provided by the sternum and rib cage in the thoracic spine.Spine (Phila Pa 1976) 30: 1283-1286.
- Chacko AG, Moorthy RK, Chandy MJ (2004) Thetranspedicular approach in the management of thoracic spine tuberculosis: a short-term follow up study.Spine (Phila Pa 1976) 29: E363-367.
- CAPENER N (1954) The evolution of lateral rhachotomy.J Bone Joint Surg Br 36-36B: 173-9.
- Benli IT, Kaya A, AcaroÄŸlu E (2007) Anterior instrumentation in tuberculous spondylitis: is it effective and safe?ClinOrthopRelat Res 460: 108-116.
- Frankel HC, Hancocck DO, Hyslop G,Melzak J, Michaelis LS, et al. (1969) The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Paraplegia. 7:179-192.
- Jensen MP, Chen C, Brugger AM (2003) Interpretation of visual analog scale ratings and change scores: a reanalysis of two clinical trials of postoperative pain.J Pain 4: 407-414.
- Mehta JS, Bhojraj SY (2001) Tuberculosis of the thoracic spine. A classification based on the selection of surgical strategies.J Bone Joint Surg Br 83: 859-863.
- Hodgson AR, Stock FE (1960) Anterior spine fusion for the treatment of tuberculosis of the spine. J Bone Joint SurgAm 42:295-310.
- Hsu LC, Cheng CL, Leong JC (1988) Pott's paraplegia of late onset. The cause of compression and results after anterior decompression.J Bone Joint Surg Br 70: 534-538.
- Upadhyay SS, Saji MJ, Sell P, Yau AC (1994) The effect of age on the change in deformity after radical resection and anterior arthrodesis for tuberculosis of the spine.J Bone Joint Surg Am 76: 701-708.
- Muheremu A, Niu X, Wu Z, Tian W (2015) Study on anterior and posterior approaches for spinal tuberculosis: a meta-analysis.Eur J OrthopSurgTraumatol 25 Suppl 1: S69-76.
- Verdú-López F, Vanaclocha-Vanaclocha V, Gozalbes-Esterelles L, Sánchez-Pardo M (2014) Minimally invasive spine surgery in spinal infections.J NeurosurgSci 58: 45-56.
- Varatharajah S, Charles YP, Buy X, Walter A, Steib JP (2014) Update on the surgical management of Pott's disease.OrthopTraumatolSurg Res 100: 229-235.
- Dong J , Zhang S, Liu H, Li X, Liu Y, et al. (2014) Novel alternative therapy for spinal tuberculosis during surgery: reconstructing with anti-tuberculosis bioactivity implants. Expert Opin Drug Deliv. 11:299-305.
- Singh R, Gogna P, Parshad S, Karwasra RK, Karwasra PK, et al. (2014) Video-assisted thoracic surgery for tubercular spondylitis.Minim Invasive Surg 2014: 963497.
- TosunB ,Erdemir C, Yonga O, Selek O (2014) Surgical treatment of thoracolumbar tuberculosis: a retrospective analysis of autogenous grafting versus expandable cages. Eur Spine J. 23:2299-2306.
- World Health Organization Global tuberculosis con¬trol: WHO report 2011 (2011) Geneva: World Health Organization.
- Rural Health Statistics in India 2012 (2012) Statistics division, Ministry of Health and Family Welfare, Government of India.
- Ganapathy K (2013) Neurosurgery in India: an overview.World Neurosurg 79: 621-628.
- El Khamlichi A (2001) African neurosurgery: current situation, priorities, and needs.Neurosurgery 48: 1344-1347.
- Reddy KS , Patel V, Jha P, Paul VK , Kumar AKS, Dandona L (2011) Towards achievement of universal health care in India by 2020: A call to action.
- Gudwani A, Mitra P, Puri A, Vaidya M (2012) India Healthcare: Inspiring possibilities, challenging journey. Prepared for confederation of Indian Industry (CII).
- Liu Z, Liu J, Peng A, Long X, Yang D, Huang S (2014) One- stage posterior debridement and transpedicular screw fixation for treating monosegmental thoracic and lumbar spinal tuberculosis in adults. Scientific World J.
- Rajiv Gandhi JeevandayeeArogyaYojana (2015) RGJAY.
- Peabody J, M Rahman, P JGertler, J Mann, DO Farley, et al. (1999) Policy and Health: Implications for Development in Asia. Cambridge University Press, Cambridge, UK.
- Alothman A, Memish ZA, Awada A, Al-Mahmood S, Al-Sadoon S, et al. (2001) Tuberculous spondylitis: analysis of 69 cases from Saudi Arabia.Spine (Phila Pa 1976) 26: E565-570.
- Al-Sebai MW, Al-Khawashki H, Al-Arabi K, Khan F (2001) Operative treatment of progressive deformity in spinal tuberculosis.IntOrthop 25: 322-325.
- Boachie-Adjei O, Squillante RG (1996) Tuberculosis of the spine.OrthopClin North Am 27: 95-103.
- Faraj AA (2001) Anterior instrumentation for the treatment of spinal tuberculosis.J Bone Joint Surg Am 83-83A: 463-4.
- McLain RF, Isada C (2004) Spinal tuberculosis deserves a place on the radar screen.Cleve Clin J Med 71: 537-539, 543-9.
- Rezai AR, Lee M, Cooper PR, Errico TJ, Koslow M (1995) Modern management of spinal tuberculosis.Neurosurgery 36: 87-97.
- Abbas A, Rizvi SR, Mahesri M, Salahuddin HR (2013) Conservative management of spinal tuberculosis: initial series from pakistan.Asian Spine J 7: 73-80.
- Boachie-Adjei O, Squillante RG (1996) Tuberculosis of the spine.OrthopClin North Am 27: 95-103.
- Tuli SM (1995) Severekyphotic deformity in tuberculosis of the spine.IntOrthop 19: 327-331.
- Tuli SM (1975) Results of treatment of spinal tuberculosis by "middle-path" regime.J Bone Joint Surg Br 57: 13-23.
- Tuli SM (1969) Treatment of neurological complications in tuberculosis of the spine.J Bone Joint Surg Am 51: 680-692.
- Rezai AR, Lee M, Cooper PR, Errico TJ, Koslow M (1995) Modern management of spinal tuberculosis.Neurosurgery 36: 87-97.
- Boachie-Adjei O, Squillante RG (1996) Tuberculosis of the spine.OrthopClin North Am 27: 95-103.
- Ghadouane M, Elmansari O, Bousalmame N, Lezrek K, Aouam H, et al. (1996) [Role of surgery in the treatment of Pott's disease in adults. Apropos of 29 cases].Rev ChirOrthopReparatriceAppar Mot 82: 620-628.
- Güven O, Kumano K, Yalçin S, Karahan M, Tsuji S (1994) A single stage posterior approach and rigid fixation for preventing kyphosis in the treatment of spinal tuberculosis.Spine (Phila Pa 1976) 19: 1039-1043.
- Kim DJ, Yun YH, Moon SH, Riew KD (2004) Posterior instrumentation using compressive laminar hooks and anterior interbody arthrodesis for the treatment of tuberculosis of the lower lumbar spine. Spine 29:E275–E279.
- McLain RF, Isada C (2004) Spinal tuberculosis deserves a place on the radar screen.Cleve Clin J Med 71: 537-539, 543-9.
- Nelson CA, Zunt JR (2011) Tuberculosis of the central nervous system in immunocompromised patients: HIV infection and solid organ transplant recipients.Clin Infect Dis 53: 915-926.
- Ade S, Harries AD, Trébucq A, Ade G, Agodokpessi G, et al. (2014) National profile and treatment outcomes of patients with extrapulmonary tuberculosis in Bénin.PLoS One 9: e95603.
- Fei J, Lai Z, Bi D, Shen J, Wei W (2013) [The un-healing cause of its management after operation of thoracolumbar tuberculosis].ZhongguoGu Shang 26: 521-525.
- Chandra SP , Ramdurg SR , Kurwale N , Chauhan A , Ansari A , et al. (2014) Extended costotransversectomy to achieve circumferential fusion for pathologies causing thoracic instability. Spine J 14:2094-2101.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences